The Untapped Potential of a Century-Old Treatment: Reviving Low-Dose Radiation Therapy for Osteoarthritis

By: David Grew MD MPH
“There is a common misconception that radiation is dangerous at any dose.”
∗ ∗ ∗
Coming up through the US medical education and training system, you can’t avoid getting hard-wired to follow the fold and support the status quo. Challenging incumbents comes with major reputational risk among your peers and future employers. Unfortunately, this can lead to stale, unimaginative practice patterns - a defensive posture unconsciously designed for self-preservation.
Sounds dramatic, but this is my best explanation for why the US, unlike most of the developed world, has not adopted a simple, low-cost treatment for osteoarthritis that is virtually side-effect-free.
Let’s take a closer look at the problem of osteoarthritis (OA). It’s a debilitating joint disease that affects 32.5 million Americans, most commonly impacting the hands, knees, and hips. OA is the leading cause of disability in the US. And as our population ages the proportion of Americans who experience years living with disability from arthritis is climbing.
Traditionally OA is treated with pain medications, steroid injections, and eventually joint replacement surgery. However, these approaches typically provide temporary relief and can carry significant risks. Some patients cannot tolerate the side effects of medicines, may not be medically fit for surgery, or simply refuse surgery outright.
For them, low-dose radiation may be a reasonable treatment option. It’s not new - the first paper describing radiation causing complete pain control in patients with arthritis was published in 1898! In fact, improvement in joint pain was one of the first documented medical benefits of radiation.
So why hasn’t low-dose radiation for OA taken off? Probably a combination of reasons. One of the primary drivers is undoubtedly a pervasive radiophobia in both the patient and healthcare provider communities. There is a common misconception that radiation is dangerous at any dose. And so using it electively for a non-cancerous condition like OA is unappealing.
Further, historically, there has not been consensus around the risks of radiation. However many experts now argue that the risks of radiation at low doses have been dramatically overestimated. Historically, the great feared risk of radiation is the creation of a new cancer. In one study, authors estimated the risk of cancer from low-dose radiation to a joint is approximately equivalent to getting a CT scan of your abdomen. In Germany, where every year thousands of patients receive radiation as a standard treatment for OA, there have been no reported cases of cancer.
Radiation Oncologists like me might also turn the spotlight inward since we’ve likely also contributed to slow adoption. Over the last two decades, there have been head-spinning advancements in radiation technology, giving us access to new tools that allow us to bend and shape radiation to precisely target difficult-to-reach cancers - improving cure rates and reducing side effects. So most of the energy and enthusiasm in the field has (rightly) been directed at leveraging our cool tech, with little room reserved for exploring the basic techniques used to treat OA.
Finally, the mainstream treatments for OA are abundantly available, reducing the perceived need for low-dose radiation. Oral medications like NSAIDS are cheap and easy to find. And these days patients are walking just hours after hip replacement surgery, many times going home the same day.
But millions of Americans don’t fit into either of these buckets. And for them, low-dose radiation may be a good option. Good candidates are older, at least over age 40, and have stopped responding to a first-line treatment like medical therapy or steroid injections.
The treatment requires a consultation with a radiation oncologist, a mapping procedure with a CT scan to design the radiation treatment, and 6 treatment visits, usually 10 minutes apiece. There is no hospitalization, all treatments are delivered, outpatient. There are virtually no side effects, although some patients have reported temporary mild skin redness in the treated area.
In terms of results, there’s a range of success rates reported but patients can reasonably expect an 80% chance of significant improvement in pain. For those who do not have a good response, or if pain returns, they can undergo a second course of radiation and expect about 60% improvement in pain.
Radiation for arthritis is generally covered by insurance, so long as doctors and clinics use appropriate (read: cheaper) technology when they bill the procedure. However, patients are responsible for typical co-pays and should check with their insurance carrier before starting treatment.
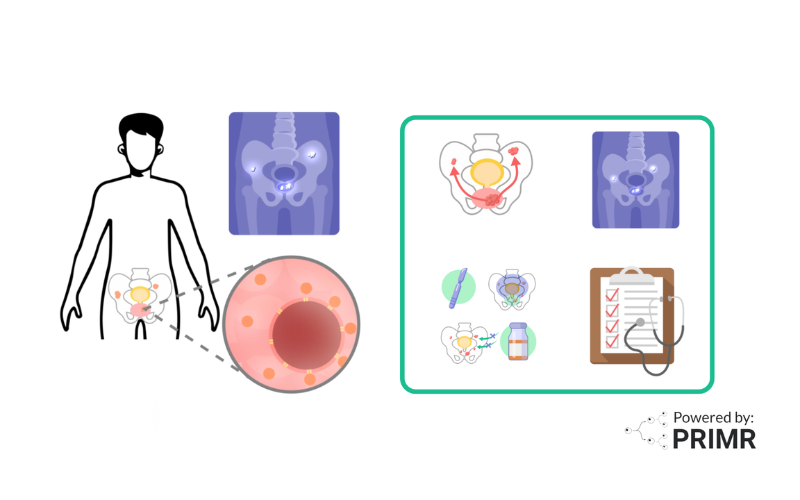
Since the subject of radiation for arthritis can be overwhelming or confusing for patients, we made a video with some simple visuals to help people understand the treatment.
As always, this is not medical advice. Talk to your doctor before making any medical decisions!
FAQs:
Is low-dose radiation therapy safe for treating osteoarthritis?
One of the primary concerns around using low-dose radiation therapy (LDRT) for osteoarthritis is the safety of radiation exposure. However, the available evidence suggests that LDRT is a very safe treatment option:
- The radiation doses used for LDRT are extremely low, typically equivalent to the amount of background radiation a person would be exposed to over a few months.
- Multiple studies have shown no increased risk of cancer or other adverse effects in patients receiving LDRT for osteoarthritis, even after long-term follow-up.
- In countries like Germany where LDRT has been used for decades to treat osteoarthritis, there have been no reported cases of radiation-induced cancers.
- The benefits of pain relief and improved joint function greatly outweigh the negligible risks associated with low radiation exposure.
How effective is low-dose radiation therapy for treating osteoarthritis?
The available research indicates that LDRT can be highly effective in managing the symptoms of osteoarthritis:
- Studies have reported significant improvements in pain, joint mobility, and quality of life in 70-80% of patients treated with LDRT.
- For those who do not respond to the initial course of LDRT, a second treatment can lead to an additional 60% improvement in symptoms.
- The pain relief and functional benefits of LDRT have been shown to last for several years in many patients.
- LDRT is particularly useful for patients who cannot tolerate or do not respond well to other standard treatments like medications or steroid injections.
Is low-dose radiation therapy covered by insurance?
In most cases, LDRT for the treatment of osteoarthritis is covered by insurance, though patients may be responsible for typical co-pays and deductibles:
- As long as healthcare providers use appropriate, cost-effective technology when billing for the LDRT procedure, it is generally considered a covered treatment.
- Patients should check with their insurance provider to understand the specific coverage details and any out-of-pocket costs they may incur.
- Some insurance companies may require prior authorization or have specific guidelines around the use of LDRT for osteoarthritis, so it's important for patients to discuss this with their provider.
- In cases where insurance coverage is limited, there may be options for financial assistance or payment plans to make LDRT more accessible.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care