AMPLIFY Trial: Advancing Imaging for Prostate Cancer Recurrence
By: David Grew MD MPH
"What makes it unique is its ability to stay detectable in the body longer."
∗ ∗ ∗
As a radiation oncologist, I often meet patients who come back after completing treatment for prostate cancer with a worried question: “Doc, my PSA levels are going up again, does this mean the cancer is back?”
This is one of the most challenging situations in prostate cancer care. A rising PSA after initial treatment—whether surgery, radiation, or another therapy—can be an early signal that the cancer has returned. But pinpointing exactly where the cancer is can be difficult, especially when it’s too small to show up clearly on standard imaging.
This is where research trials like AMPLIFY are so important. They test new imaging tools that could help us detect recurrence earlier and with greater accuracy, ultimately guiding us toward more effective treatments.
Why PSA Levels Matter After Treatment
PSA, or prostate-specific antigen, is a protein normally produced by the prostate gland. After initial prostate cancer treatment, doctors use PSA levels as a marker to monitor how well the treatment worked. Ideally, PSA levels drop to very low levels and stay there.
But when PSA starts rising again, it suggests that prostate cancer cells may still be active in the body. The challenge is figuring out where those cells are, whether they’ve remained in the prostate area or spread to lymph nodes, bones, or elsewhere. Traditional imaging tools like CT or MRI can sometimes identify spread, but they often miss small or early lesions. That gap can mean delayed treatment or less tailored care.
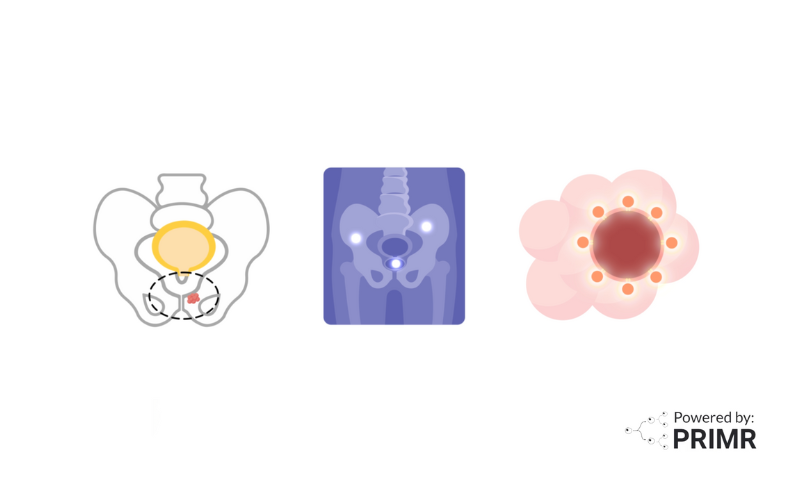
The Role of PSMA PET Scans
In recent years, PSMA PET scans have become a powerful tool in prostate cancer imaging. They work by using a radioactive tracer that binds to PSMA, a protein found in high amounts on prostate cancer cells. Once injected, the tracer highlights areas of cancer spread, making them visible on PET scans.
Compared to conventional imaging, PSMA PET scans are more sensitive at detecting cancer. They can detect cancer in lymph nodes, bones, or distant sites that would otherwise go unnoticed. This accuracy not only confirms whether recurrence is happening but also helps doctors tailor treatments—avoiding unnecessary therapies in some cases while guiding more aggressive approaches in others.
Still, even current PSMA tracers have limits. They may miss very small tumors or have a narrow time window for imaging, meaning some opportunities for detection could be lost. That’s where the AMPLIFY trial comes in.
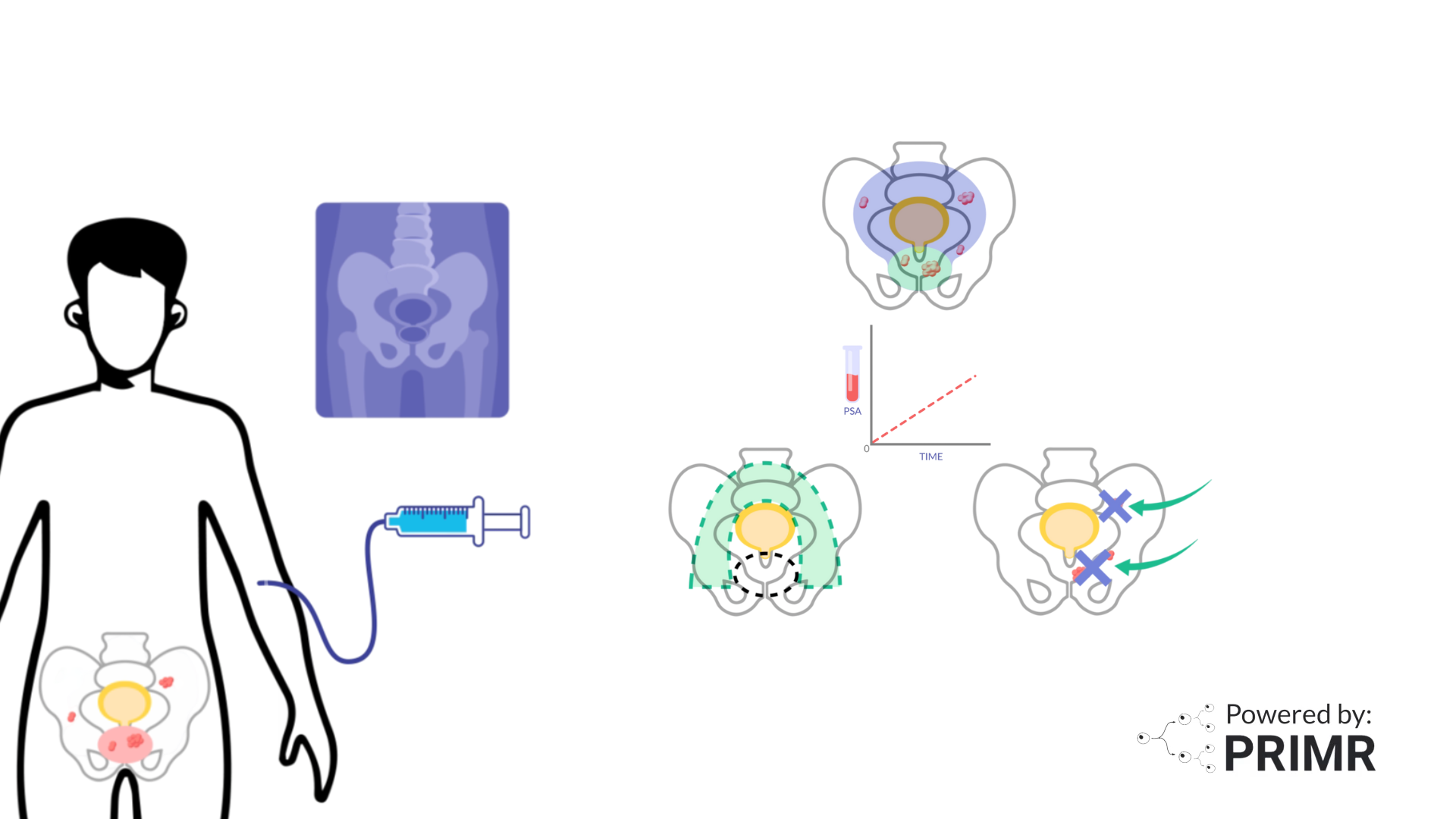
The AMPLIFY Trial and ⁶⁴Cu-SAR-bisPSMA
The AMPLIFY trial is evaluating a new investigational imaging agent, ⁶⁴Cu-SAR-bisPSMA, designed to improve upon existing PSMA tracers. What makes it unique is its ability to stay detectable in the body longer. This allows doctors to capture images at both early time points (around 1–4 hours) and later time points (around 24 hours) after injection.
This extended window could offer several advantages:
- Improved accuracy: making it easier to see small or hidden areas of recurrence.
- More flexibility: giving patients and clinics more options for scheduling scans.
- Better treatment planning: allowing doctors to see the full extent of cancer spread and make more informed decisions about surgery, radiation, or systemic therapies.
Patients enrolled in the AMPLIFY trial receive the tracer, undergo PET/CT scans at both time points, and have their results compared with clinical follow-ups or additional tests. This helps determine not only whether the cancer has returned, but also how effective ⁶⁴Cu-SAR-bisPSMA is compared to current imaging options.
What This Could Mean for the Future
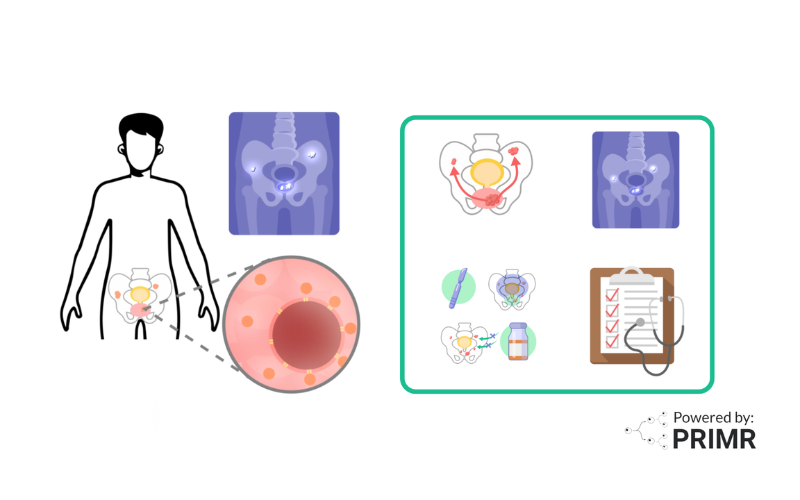
The potential of the AMPLIFY trial goes beyond just sharper images. If ⁶⁴Cu-SAR-bisPSMA proves to be more accurate, it could redefine how doctors manage prostate cancer recurrence.
For patients, this could mean:
- Detecting recurrence earlier, when treatments are more effective.
- Avoiding unnecessary or misdirected treatments by knowing exactly where cancer is.
- Receiving truly personalized care, based on precise knowledge of disease spread.
The broader impact could be even greater. Tools like this may one day influence how we approach not just prostate cancer, but other cancers where early detection of recurrence is critical.
—
The AMPLIFY trial highlights an exciting step forward in prostate cancer imaging. By refining how we detect recurrence, we move closer to offering patients treatments that are more accurate, timely, and effective.
For patients with prostate cancer—and even for those with other cancers, like lung cancer—research like this gives us hope. Each advancement in imaging brings us closer to catching disease earlier, tailoring treatments better, and improving outcomes. That’s a future worth striving for.
To learn more about the AMPLIFY clinical trial, watch the video we made here.
To learn more, browse our library of prostate cancer-related topics.
Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
How early could ⁶⁴Cu-SAR-bisPSMA detect recurrence compared to current PSMA scans?
One of the main hopes for this new tracer is that it can spot tiny clusters of cancer cells earlier than the tracers doctors currently use. If recurrence is caught sooner, patients may be eligible for treatments while the cancer is still limited and easier to control. This could make a real difference in long-term outcomes.
Could this imaging agent reduce the need for repeated or unnecessary treatments?
Many men with rising PSA but unclear scans end up receiving broad treatments like hormone therapy, even when the exact cancer location isn’t known. A more accurate scan could help doctors target only the areas that truly need treatment, sparing patients from unnecessary side effects. This approach could also save time and healthcare costs by preventing overtreatment. In the long run, better precision may improve both quality of life and treatment effectiveness.
Will ⁶⁴Cu-SAR-bisPSMA work equally well for all prostate cancer patients?
Not every patient’s cancer behaves the same way. Some aggressive forms of prostate cancer may produce less PSMA, making them harder to detect even with advanced tracers. Researchers are still studying whether ⁶⁴Cu-SAR-bisPSMA performs better across different prostate cancer subtypes. If proven effective for a wider range of patients, it could become a new standard tool for monitoring recurrence.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care