Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
.png)
By: David Grew MD MPH
"For patients, this means a growing number of options when standard therapies are no longer enough."
∗ ∗ ∗
As a radiation oncologist, I’m often asked by patients about new treatment options, especially when standard therapies no longer seem to work. I remember one patient asking me, “Doc, if the cancer doesn’t respond to chemotherapy or hormone therapy, what else can be done?”
That’s where the exciting field of PSMA treatment comes in. Research into prostate cancer is constantly evolving, and one of the most promising advances we’ve seen in recent years is the development of PSMA-targeted therapies. These therapies not only change how we diagnose prostate cancer but also how we treat it, offering hope for patients with advanced disease.
Understanding PSMA and Why It Matters
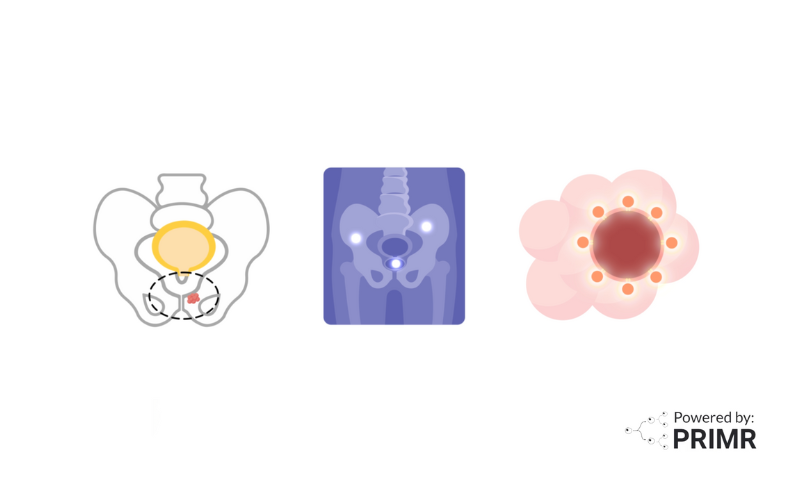
PSMA stands for Prostate-Specific Membrane Antigen, a protein found in especially high amounts on prostate cancer cells. While normal tissues also produce PSMA, prostate cancer cells carry much more of it. This makes PSMA an excellent “flag” for doctors to find and treat cancer.
Scientists have taken advantage of this by creating special molecules that can attach to PSMA. When combined with a radioactive drug (known as a radiopharmaceutical), these molecules deliver radiation directly to the cancer cells. This approach is called PSMA-targeted radioligand therapy (PSMA-RLT).
How PSMA Treatment Works
PSMA treatment works differently from traditional cancer treatments like chemotherapy or external beam radiation. Instead of treating broad areas of the body, PSMA therapy is highly selective:
- Targeting Cancer. A radioactive drug is injected into the bloodstream. This drug travels through the body and attaches to PSMA proteins on prostate cancer cells.
- Delivering Precision Radiation. Once attached, the radioactive component delivers radiation directly to the cancer cells, damaging their DNA so they can’t grow or spread.
- Sparing Healthy Tissues. Because PSMA is far less common in normal cells, the therapy minimizes damage to healthy tissue. This makes it especially valuable for patients whose cancer has spread beyond the prostate.
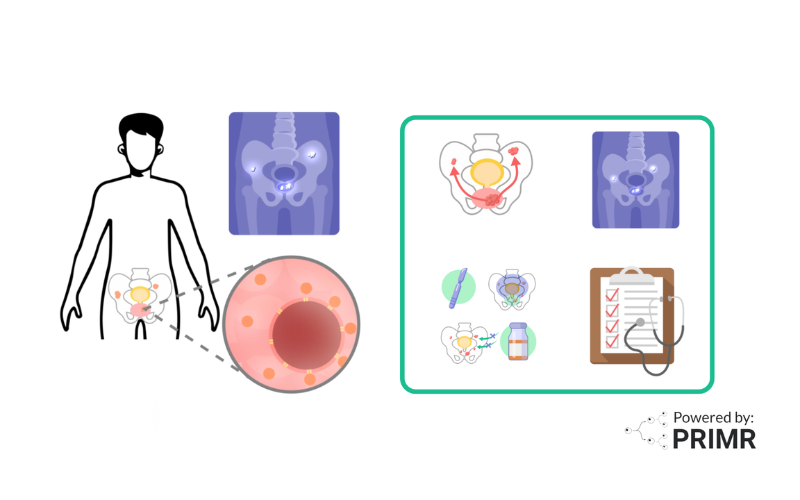
Who is Eligible for PSMA Treatment?
PSMA treatment is generally used in men with advanced prostate cancer that has spread outside the prostate and is no longer responding to hormone therapy, this stage is called metastatic castration-resistant prostate cancer (mCRPC).
Before beginning treatment, doctors often order a PSMA PET scan to confirm whether the cancer cells are expressing PSMA. If the scan shows strong PSMA activity, the patient may be a candidate for PSMA therapy. Typically, these patients may have already tried chemotherapy or hormone therapy but need a new approach to control their disease.
Benefits and Potential Side Effects
The main advantage of PSMA treatment is that it directly targets prostate cancer cells. This precision can result in better tumor control, slowing or stopping disease progression and, in some cases, shrinking tumors.
However, like all treatments, PSMA therapy is not without risks. Possible side effects may include dry mouth, fatigue, nausea, loss of appetite, urinary tract infections, bowel changes, or low blood counts. In rare cases, kidney damage or infertility may also occur. Because of this, doctors carefully monitor patients during and after treatment, adjusting care as needed to manage side effects.
Looking Ahead: The Future of PSMA Therapy
PSMA treatment is still an evolving field, and research is underway to make it even more effective. Some studies are combining PSMA therapy with hormone therapy, while others are developing new drugs to increase accuracy and reduce side effects. These advances are pushing cancer care into an era of more personalized and targeted treatments.
For patients, this means a growing number of options when standard therapies are no longer enough. And while PSMA treatment today is most widely studied in prostate cancer, the research surrounding targeted therapy continues to inspire new possibilities, even for other cancers like lung cancer, where precision approaches could dramatically improve outcomes in the future.
–
PSMA treatment represents a new way forward in cancer care, one that uses precision targeting to fight prostate cancer more effectively and with less damage to healthy tissue. For patients and doctors alike, it signals an important step in shifting cancer treatment toward approaches that are more focused, more personalized, and more hopeful.
As research expands, we may soon see PSMA therapy, or therapies like it, playing a role not only in prostate cancer but in other hard-to-treat cancers as well. And for patients facing advanced disease, including those with lung cancer, these breakthroughs hold a very real promise: that better treatments are not only possible but already on the horizon.
To learn more about PSMA Treatment, watch the video we made here.
To learn more, browse our library of nuclear medicine and prostate cancer-related topics.
Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
How long does PSMA treatment usually work before the cancer grows again?
For many men with advanced prostate cancer, PSMA therapy can keep the disease under control for months to sometimes over a year, depending on how aggressive the cancer is and how well the treatment is tolerated. Studies like the VISION trial showed that patients lived longer and had slower disease progression compared to those who received only standard care. Still, responses vary, and eventually, most cancers develop resistance. Doctors are now studying combination treatments to make the benefits of PSMA therapy last even longer.
Can PSMA therapy be used earlier in the course of prostate cancer?
Currently, PSMA therapy is mostly used when the cancer has stopped responding to hormone treatments and has spread. However, ongoing trials are testing whether using it earlier, such as before or after chemotherapy, or even in newly diagnosed high-risk patients, could improve long-term outcomes. Early results suggest that starting PSMA treatment sooner may control cancer more effectively, but doctors are waiting on larger trials before making it part of standard care. If proven, this could shift treatment strategies significantly.
What happens if a patient does not respond to PSMA therapy?
Not all patients benefit from PSMA treatment, especially if their cancer cells don’t produce enough PSMA proteins for the drug to attach to. In these cases, doctors may recommend other therapies such as chemotherapy, immunotherapy, or participation in clinical trials exploring new drugs. Some studies are testing next-generation PSMA agents designed to work even when PSMA levels are low. This highlights why PSMA PET scans are so important in deciding who is most likely to benefit before treatment begins.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care