Nuclear Medicine: Understanding PSMA and Its Role in Cancer Care
By: David Grew MD MPH
"Doctors and researchers have learned to use this protein to both visualize and treat cancer more effectively."
∗ ∗ ∗
As a radiation oncologist, one of the most common experiences I’ve had is patients asking about the newest ways we can find or treat cancer more precisely.
For instance, I remember a caregiver who came to me, frustrated after their patient had already undergone several scans and treatments, only to ask: “Doc, is there a test that can really show if the cancer is hiding somewhere we missed?” Questions like this highlight why ongoing trials and advances matter so much.
One area of exciting progress involves something called PSMA, or Prostate-Specific Membrane Antigen. Although it’s most well-known in prostate cancer care, research into PSMA has already reshaped how we approach imaging and treatment. It also gives us a glimpse into what may one day be possible for other cancers, such as lung cancer.
What is PSMA?
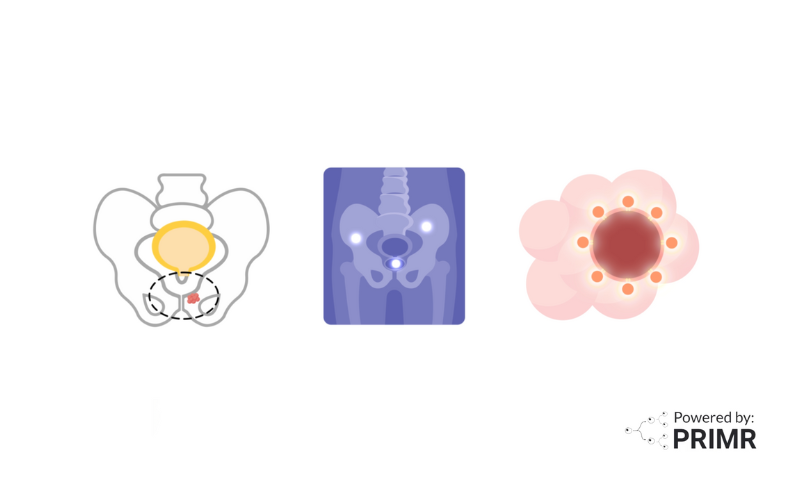
PSMA is a protein found at much higher levels on the surface of prostate cancer cells than on most normal cells. Because of this, it serves as a sort of “flag” that makes prostate cancer cells easier to identify and target. Doctors and researchers have learned to use this protein to both visualize and treat cancer more effectively.
In practice, PSMA has become a powerful tool in two main ways:
- Imaging: helping us see cancer through specialized scans.
- Treatment: allowing therapies to target cancer cells directly.
How PSMA is Used in Imaging
One of the most important applications is in PSMA PET scans. A PET scan, or Positron Emission Tomography scan, is a specialized imaging test that creates 3D images of the body. Before the scan, a patient receives an injection of a radiopharmaceutical, a small dose of a radioactive drug, that attaches itself to PSMA proteins on cancer cells.
When the scan is performed, areas with high PSMA activity light up, showing doctors exactly where prostate cancer cells may be hiding. This can reveal not only whether cancer is present in the prostate but also whether it has spread to lymph nodes, bones, or other organs. For patients, this often means greater certainty about the extent of their disease, and for doctors, it means more confidence in choosing the right treatment.
How PSMA is Used in Treatment
Beyond helping us see cancer, PSMA can also be used to treat it. In a newer approach known as PSMA-targeted radioligand therapy (RLT), a radioactive drug is designed to bind directly to PSMA proteins on cancer cells. Once attached, the drug delivers radiation specifically to those cells, killing them while sparing much of the healthy tissue around them.
This approach is especially promising for patients with advanced or metastatic prostate cancer, where treatment options may be limited. While it does carry risks like any cancer therapy, PSMA-targeted treatments represent an important step toward therapies that are both effective and more precise.
Why PSMA Matters in Prostate Cancer Care
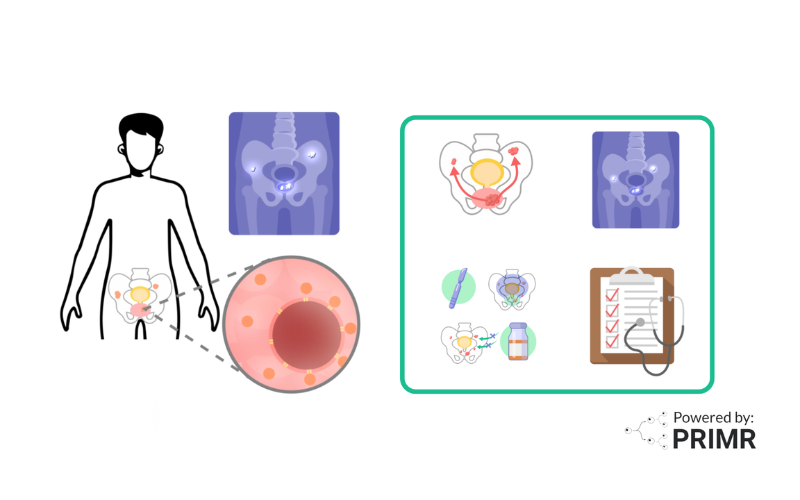
PSMA has quickly become central to modern prostate cancer care because it can help at multiple stages:
- Early detection: Identifying cancer earlier or spotting recurrence after treatment.
- Tracking spread: Showing where cancer has metastasized, so treatment can be better planned.
- Guiding treatment: Allowing therapies to target PSMA, bringing radiation directly to cancer cells.
Together, these uses give patients a better chance of receiving care tailored to their specific situation, whether that means catching cancer early, refining treatment decisions, or providing new therapeutic options when others have been exhausted.
–
The story of PSMA is a powerful example of how advances in science can change the landscape of cancer care. Right now, its greatest impact is in prostate cancer, where it has already improved how we diagnose, stage, and treat the disease. But discoveries like these remind us that the tools we develop for one type of cancer can open doors for others.
For patients with lung cancer and other cancers, PSMA research gives hope. It shows us that by learning how to better see and target cancer at the molecular level, we are moving closer to a future where treatments are more precise, less invasive, and ultimately more effective.
To learn more about PSMA, watch the video we made here.
To learn more, browse our library of nuclear medicine and prostate cancer-related topics.
Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
How do doctors decide which patients are candidates for PSMA-based care?
Not every patient with prostate cancer automatically qualifies for PSMA scans or therapies. Doctors usually recommend them for men with high-risk disease, those whose cancer has spread, or patients whose cancer has come back after surgery or radiation. Eligibility may also depend on how much PSMA protein is seen on a patient’s tumor during initial imaging. Clinical trials are helping to refine these guidelines so that PSMA use is targeted to the patients most likely to benefit.
Could PSMA approaches work for cancers other than prostate cancer?
Researchers are actively exploring whether PSMA-targeted imaging and therapies can help in cancers such as lung, kidney, or certain types of salivary gland tumors where PSMA is sometimes present. Early studies show promise, but these uses are not yet routine. If successful, PSMA could one day become part of precision medicine for multiple cancers, opening the door to more tailored treatments beyond prostate cancer.
How widely available is PSMA imaging and treatment right now?
While PSMA PET scans and PSMA-targeted therapies have been approved in several countries, including the United States, they are not accessible in all hospitals or regions. Access often depends on specialized equipment and trained staff, as well as whether insurance covers the test or treatment. Many patients may need to travel to larger cancer centers to receive PSMA-based care. Expanding access remains a major focus for the cancer community so that more patients can benefit.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care