Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care
By: David Grew MD MPH
"The biggest strength of PSMA imaging is accuracy."
∗ ∗ ∗
As a radiation oncologist, one of the most common questions I hear from patients is: “How do you know if the cancer has spread?” It’s a deeply personal and important question because the answer guides every step of treatment planning.
I recall a patient who had undergone surgery for prostate cancer but later saw his PSA levels rising again. His biggest concern was whether the cancer had returned, and if so, where. This is exactly the kind of situation where advanced imaging, like PSMA PET scans, can make a difference.
Understanding the tools we use to see cancer more clearly is essential not only for doctors but also for patients making decisions about their care. One of the most promising advances in prostate cancer imaging is PSMA-targeted PET imaging, or simply PSMA imaging.
What is PSMA Imaging?
To understand PSMA imaging, it helps to first know what PSMA is. PSMA stands for Prostate-Specific Membrane Antigen, a protein found in high amounts on the surface of prostate cancer cells. By targeting this protein, doctors can see cancer much more clearly than with conventional scans like CT or MRI.
PSMA imaging is performed using a PET scan (Positron Emission Tomography). Before the scan, a patient is injected with a small amount of a radioactive drug, called a radiopharmaceutical, that specifically binds to PSMA on prostate cancer cells. Once injected, the tracer travels through the body, attaches to cancer cells, and lights them up on the scan. This allows doctors to see exactly where the cancer is located and whether it has spread.
The process usually involves three key parts:
- Injection of the tracer. The patient receives a radiopharmaceutical designed to bind to PSMA proteins on cancer cells. Different tracers exist, and one important factor is their “half-life,” which affects how long they stay active in the body.
- The scan itself. After a short wait, the patient undergoes a PET/CT or PET/MRI scan. The PET portion detects the tracer bound to cancer cells, while CT or MRI provides detailed structural images. Together, these create a highly accurate picture of cancer in the body.
- Doctor review and analysis. Specially trained doctors then interpret the images, determining whether the cancer is localized or has spread. These results play a direct role in treatment planning.
How is PSMA Imaging Used in Prostate Cancer Care?
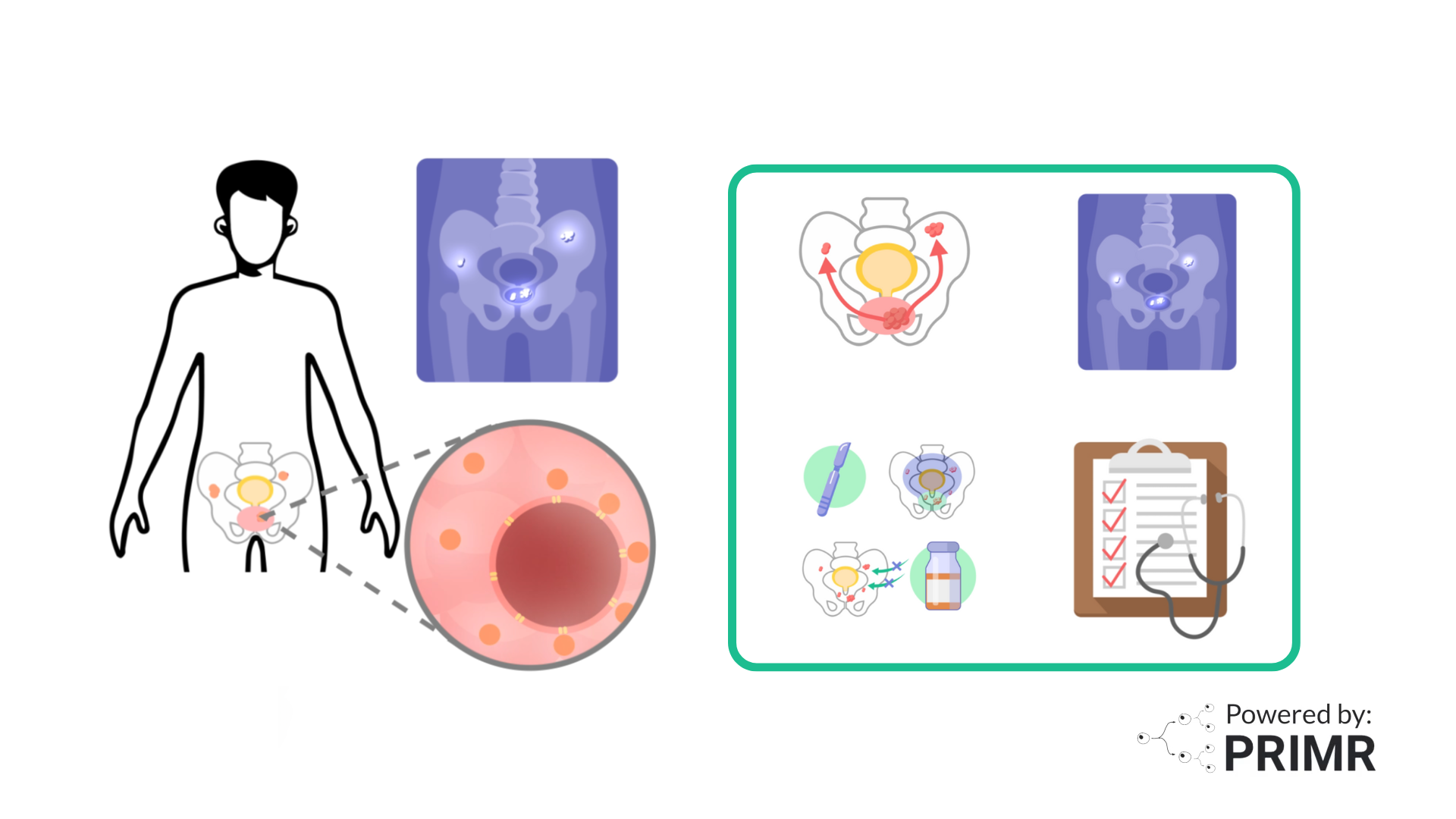
PSMA imaging can be used at different stages of prostate cancer management:
- Diagnosis and staging. It helps determine whether the cancer is confined to the prostate or has spread to nearby lymph nodes, bones, or distant organs.
- Treatment planning. The accuracy of PSMA imaging allows doctors to tailor treatments, whether that’s surgery, radiation, systemic drug therapy, or targeted PSMA therapies such as radioligand therapy (RLT).
- Detecting recurrence. If PSA levels rise after treatment, PSMA scans can identify whether the cancer has returned and where, guiding the next steps.
- Monitoring response. Doctors can also use PSMA imaging to check how well a patient’s treatment is working, ensuring care remains on the right track.
Benefits of PSMA Imaging
The biggest strength of PSMA imaging is accuracy. Traditional imaging sometimes misses small or hidden tumors, but PSMA PET scans can highlight cancer cells with much greater clarity. This accuracy allows for better staging, more confident treatment decisions, and fewer unnecessary procedures.
By providing a more complete picture of prostate cancer, PSMA imaging empowers both doctors and patients. It allows care to be personalized, giving each patient the best possible chance of receiving the right treatment at the right time.
Who Can Benefit from PSMA Imaging?
PSMA imaging is most often used for:
- Patients with newly diagnosed prostate cancer who are considered intermediate- or high-risk.
- Men whose PSA levels rise after initial treatment, suggesting the cancer may have returned.
- Patients who may be candidates for PSMA-targeted therapies, which depend on confirming PSMA expression in cancer cells.
Ultimately, whether PSMA imaging is right for a patient depends on their specific situation. The decision is made in close consultation between the patient and their care team.
–
PSMA imaging represents a significant step forward in cancer detection and management, particularly in prostate cancer. By allowing us to see cancer with greater accuracy, it has the potential to improve how we diagnose, treat, and monitor the disease.
And while this technology is currently focused on prostate cancer, advances in imaging continue to influence research across many cancer types. For patients facing cancers like lung cancer, developments like this offer real hope that more precise tools will continue to improve the way we detect and fight cancer in the years ahead.
To learn more about PSMA Imaging, watch the video we made here.
To learn more, browse our library of nuclear medicine and prostate cancer-related topics.
Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
Does PSMA imaging replace standard scans like CT or MRI?
PSMA imaging is more sensitive and accurate, but it doesn’t completely replace CT or MRI. In most cases, doctors use PSMA PET scans alongside these traditional imaging tools because each provides different types of information. For example, CT and MRI give detailed pictures of anatomy, while PSMA scans highlight cancer cells specifically. Using both together gives the clearest view of the disease, ensuring that nothing important is missed in treatment planning.
What are the risks or downsides of PSMA imaging?
PSMA imaging is generally safe, but like any test involving radiation, there is a small amount of exposure. The radioactive tracer usually leaves the body within a day, and side effects are rare, though some patients may experience mild discomfort at the injection site. Another consideration is that PSMA scans can sometimes pick up benign conditions, like inflammation, that also show PSMA activity, which could lead to false positives. This is why results always need to be interpreted by experienced specialists who can put the findings into context.
How might PSMA imaging change treatment outcomes in the long run?
Studies have shown that PSMA imaging can detect cancer that other scans miss, which often changes how doctors approach treatment. For example, it can help avoid unnecessary surgeries in men whose cancer has already spread, or it can direct radiation more precisely to where cancer cells are hiding. Over time, this could mean fewer side effects from overtreatment and better survival outcomes. Ongoing research will show just how much PSMA imaging improves long-term results, but early evidence is very promising.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care