Navigating the Evolving Landscape of Informed Consent in Clinical Trials: Draft FDA Guidance and the PRIMR Approach

By: David Grew MD MPH
“I started building PRIMR because I thought there was a better way to teach patients about clinical trials.”
∗ ∗ ∗
I’ve had countless conversations with patients, PIs, and clinical trial site staff lamenting the miserable state of informed consent processes for clinical trials. How could a 40-page document in legalese possibly be a solution that makes sense? It doesn’t work for anybody. Patients don’t understand it, PIs don’t have time to walk patients through it, and site staff don’t always have the background needed to field the array of clinical questions that inevitably come up during the process.
Full disclosure: this is one of our longer blogs, but I promise I tried to make it super value-dense. Please stick with it - you will learn things!
I started building PRIMR because I thought there was a better way to teach patients about clinical trials. I could see the frustration on my own patients' faces when they tried to comprehend their complex cancer problem and the available trial options. Likewise, I understood the pain of my colleagues who are PIs or sponsors that need to build a standardized good explanation for their trial and scale it across all enrolling sites.
I began by helping clinical trial teams turn ICFs into short 2-3 minute scripts in lay language. Then, I recorded narration with a clinician’s tone - confident with the subject matter but not too sales-y to tip into cringeworthy coercive territory. Finally, I built a team of medical graphic designers to bring the explanation to life with simple, easy-to-follow motion graphics.
The positive response has been incredible, and our team knows we’re just getting started. But there’s loads of work to be done. I think every clinical trial should come with a PRIMR-like trailer so eligible participants can quickly and easily understand their trial options by consuming short-form video. This is how we consume content and learn in our spare time, why should patient education be different?
So when the FDA recently published draft guidance on how clinical trial sponsors can make the informed process more patient-centric – I busted out the popcorn and dove in. While PRIMR doesn’t build consent forms, we do build educational content eligible participants consume during the consent process.
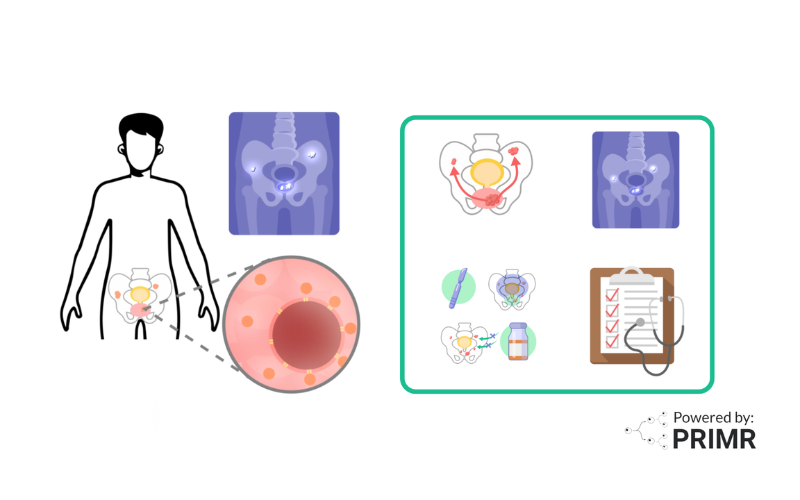
In this blog, we'll delve into key points from recent FDA guidance and highlight how PRIMR, a pioneering patient education company, is at the forefront of facilitating patient understanding in complex oncology clinical trials.
Informed Consent: The Highlights From New Draft FDA Guidance
The recent draft FDA guidance, though not legally binding, may help IRBs, investigators, and sponsors in improving participant comprehension. This draft guidance is open to public comment and is not yet final. Below are some of the key points I found useful, as well as how PRIMR is positioned to execute top-notch educational products for clinical trial sponsors.
The Key Information Section
The FDA likes consents to start with a short section - the Key Information Section - ahead of the more detailed, deeper dive consent document. This section gives eligible participants a high-level preview of what’s to come. Most of the recommendations in the draft guidance apply to how sponsors can leverage this key information section of the consent to improve patient understanding and overall experience. Here are some elements they recommend including.
PRIMR’s Approach: A high-level overview of complex clinical trials is our whole reason for existence. We build content to make things easy for anyone to understand - whether you have a 5th-grade education or you’re a physician considering referring a patient for enrollment on a trial. Look no further than the H1 on our home page: “Simple Cancer Explanations.”
Voluntary Participation and Right to Discontinue Participation
Informed consent mandates that research participants have the right to voluntary participation. It’s crucial to inform potential subjects that they can opt-out at any time without facing penalties or losing entitled benefits. Additionally, the FDA recommends reassuring patients that decisions won’t affect their relationships with healthcare providers.
PRIMR’s Approach: We always first teach patients about the standard of care treatment. It’s important to establish the foundational knowledge so patients have SOC as a reliable choice. A good example of a trial video where PRIMR first lays out standard treatment is the SAMURAI trial investigating the addition of stereotactic radiation to immunotherapy and anti-angiogenic therapy in metastatic renal cell carcinoma (see the 0:15 mark).
We have on occasion specifically mentioned that participation is not mandatory, although some sponsors feel that is implied. We may consider adding a line about this in scripts going forward. However, there are trade-offs between viewer retention and “completeness” - making a video long to talk about volunteerism may risk losing some viewers who already know and accept that fact.
Purpose of Research, Expected Duration, and Procedures to be followed
The FDA recommends describing the rationale behind the research, including factors such as the subject’s medical condition, treatment history, or responsiveness to prior interventions. It’s essential to communicate the study’s design, including any randomized investigations with placebo elements, in accessible language. Furthermore, detailing the anticipated duration of involvement, primary procedures, and involvement of investigational medical products is imperative. Clear emphasis on the time commitments, including visit frequency and duration, is warranted. When discussing investigational products, it’s vital to cover aspects such as placebo usage, randomization procedures, and post-study treatment options. Providing insights into how study care compares to standard care is also valuable.
PRIMR’s Approach: Since we’re building for the visual learner, we don’t miss an opportunity to create a graphic to explain a new drug, device, or procedure. After thousands of conversations with patients about complex therapies, we know that top-of-mind questions include how many treatment visits and how much time to expert per visit. We also address typical questions that drive long standing barriers to entry on trials, like trust and credibility - use of placebo and randomization. We again use visuals to show that there are two groups of treatments on RCTs and neither doctors nor patients get to choose which treatment they get.
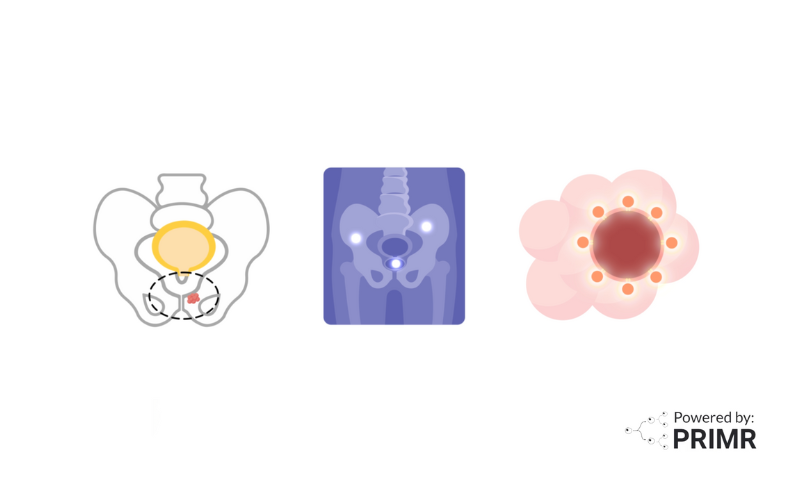
The INNOVATE prostate cancer clinical trial is a good example of a PRIMR video that addresses patient questions around rationale, study design, randomization, and placebo (the study design section starts at the 2:17 mark).
Reasonably Expected Risks and Benefits
The FDA recommends prospective subjects should be informed about any anticipated positive outcomes, both for themselves and for society (I agree!). It’s essential to communicate these benefits clearly and realistically, avoiding any overly optimistic portrayals. This includes detailing any direct impact on the participant’s health condition or illness. For instance, if a clinical trial aims to assess whether an investigational medical product can reduce tumor size, it’s important to highlight the uncertainty surrounding its effectiveness and its potential implications for the participant’s quality or length of life. Additionally, prospective subjects should be made aware that research differs from clinical care, and there may be considerable uncertainty regarding the benefits. Therefore, any potential benefits should be presented in simple and straightforward terms to ensure informed decision-making.
Assessing risks and discomforts is a crucial aspect of informed consent in research participation as well. It’s vital to prioritize and clearly communicate the most common and serious risks associated with the study, including those related to investigational medical products or research procedures. This information should be easily accessible, ideally presented on the first page of the key information section. While it may not be feasible to list all foreseeable risks, interested parties should ensure that prospective subjects understand the possibility of unknown risks and the potential lack of improvement or exacerbation of their condition. Distinguishing between risks associated with investigational products/procedures and those associated with other research interventions is important. Additionally, the key information section may include details about actions taken to monitor and mitigate risks throughout the research process, such as safety monitoring or dose adjustments.
PRIMR’s Approach: In the METANOVA trial, patients can receive stereotactic ablative radiation to up to ten (!) sites of metastatic disease. That is not standard. But may be beneficial. So patients who enroll will get access to a therapy that is otherwise unavailable off-trial (see the 2:35 mark). In addition, for all our trials, we like to mention that a key potential benefit of enrolling is helping future patients with cancer receive better care based on the things doctors learn from participants on the trial.
In the FRONTIER trial, patients with recurrent glioblastoma receive microscopic radioactive glass beads. The treatment requires an angiogram: procedure and has clear risks over the standard of care. See how we addressed those risks in the video at the 1:52 mark.
Organization and Presentation of the Consent Materials
The guidelines emphasize the importance of presenting information in a manner that aids comprehension rather than overwhelming it with isolated facts. One suggested method is to utilize “bubbles,” visually organizing key information within defined borders to enhance readability. Research has shown that such formats improve comprehension, particularly when information is simplified and grouped.
Beyond the key information section, the entire consent form should follow plain language principles, prioritizing clarity and simplicity. Organizing the document thoughtfully, possibly employing a tiered approach for complex studies, can further enhance understanding. Additionally, using understandable language and considering the characteristics of the prospective subjects’ population, such as age and language proficiency, are crucial for effective communication. Regular review by individuals unfamiliar with the research can also ensure that the consent materials facilitate understanding, ultimately promoting ethical and informed participation in research endeavors.
PRIMR’s Approach: This was perhaps the most welcome section of the guidance for me. We use white space background as a way to keep things simple and draw attention to only the most important elements of our content. This idea came from the constraints of a doctor drawing out an explanation for a patient on an exam table paper. We adapted that for the screen but kept color minimal, using only primary colors for emphasis. We aim to write at the 5th-grade level. We check our scripts for jargon with the CDC lay language thesaurus and have patient advocates review our content. We also make all our content public and our growing audience of physicians and patients sometimes points out confusing elements which we then go back and correct.
In the ESCAPE trial, patients with prostate cancer who are motivated to avoid treatment can enroll in active surveillance. It is important they understand the procedures involved. There are several required tests, so to keep them straight we use white space to separate the tests into categories, aiming to improve comprehension and using simple images as memory hooks (see an example at the 0:37 mark).
In conclusion, navigating the evolving landscape of informed consent in clinical trials demands innovative solutions that prioritize patient understanding and engagement. At PRIMR, we collaborate with clinical-stage biotech, pharma, and large academic centers to develop comprehensive content solutions tailored to individual trial portfolios.
By transforming complex information into digestible formats, such as short videos and visually organized materials, we empower patients to make informed decisions about their participation. Our commitment to clarity, simplicity, and patient-centered education ensures that the informed consent process becomes not just a legal requirement, but a meaningful step towards advancing medical research and improving patient outcomes.
Work with us on your next trial: Custom Content and Strategic Distribution for Clinical Trials
FAQs:
How does PRIMR ensure that its educational content remains accessible to patients with varying levels of health literacy and educational backgrounds?
We ensure accessibility by adhering to a 5th-grade reading level, using visual aids, and consulting resources like the CDC lay language thesaurus. Additionally, patient advocates review content for clarity and jargon; audience feedback helps identify and address confusing elements.
What specific challenges does PRIMR face in translating complex clinical trial information into lay language while maintaining accuracy and comprehensiveness?
While we have a meticulous and proven process, a specific challenge for us is balancing simplicity with completeness. This entails conveying complex clinical trial information in a clear and understandable manner while ensuring that all essential details are included. This balance is crucial because overly simplified content may lack important information, leading to misunderstandings or incomplete comprehension by patients. On the other hand, overly complex content may overwhelm individuals with limited health literacy or educational backgrounds, hindering their ability to make informed decisions about participating in clinical trials.
How does PRIMR address the ethical considerations surrounding patient education in clinical trials, particularly in terms of ensuring that information is presented transparently and without coercion?
We do this by prioritizing clarity, simplicity, and patient-centered education. Transparency is key, and content is presented without coercion or bias. Patient autonomy and voluntary participation are emphasized, and the goal is to empower patients to make informed decisions about their involvement in clinical trials.
Other Posts
Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care