Nuclear Medicine: Seeing and Treating Cancer from the Inside
By: David Grew MD MPH
"For patients, it means earlier detection, more precise treatments, and potentially fewer side effects."
∗ ∗ ∗
As a practicing radiation oncologist, I often meet patients who ask questions like: “Doctor, how can you really tell if my treatment is working?” or “How do you know if the cancer has spread where the scans can’t see?” These are difficult but important questions. In many cases, the answer lies in a field of medicine that is both diagnostic and therapeutic—nuclear medicine.
Recent advances in this field have had a significant impact, particularly in clinical trials that explore new imaging agents and therapies. For example, imagine a patient with lung cancer who has already had a CT scan and an MRI. The scans may show where the tumor is, but they can’t always tell us how the cancer cells behave or whether small, hidden clusters are active in the body. That’s where nuclear medicine provides answers—and sometimes, solutions.
What is Nuclear Medicine?
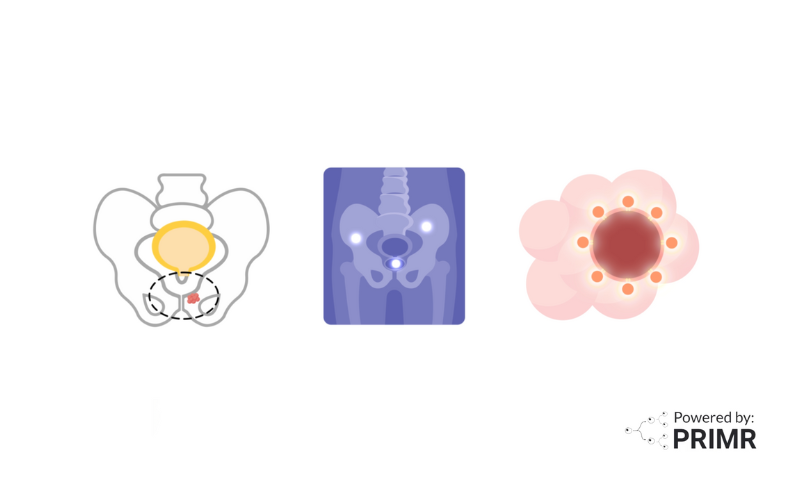
Nuclear medicine is a branch of medicine that uses radiopharmaceuticals, or radioactive drugs, to either visualize or treat disease inside the body. Unlike traditional scans such as X-rays, CT, or MRI—which show anatomy and structure—nuclear medicine looks deeper into function and biology. It can reveal how cancer cells are behaving, how organs are working, and whether certain proteins that are important for diagnosis or therapy are present.
Here’s how it works: once a radiopharmaceutical is injected into the body, it travels to its target—whether that’s a tumor, an organ, or a specific protein marker. Special cameras, such as PET (Positron Emission Tomography) or SPECT (Single Photon Emission Computed Tomography), then detect the signals released by the radiotracer and produce images that allow us to see inside the body in a way that goes beyond standard imaging.
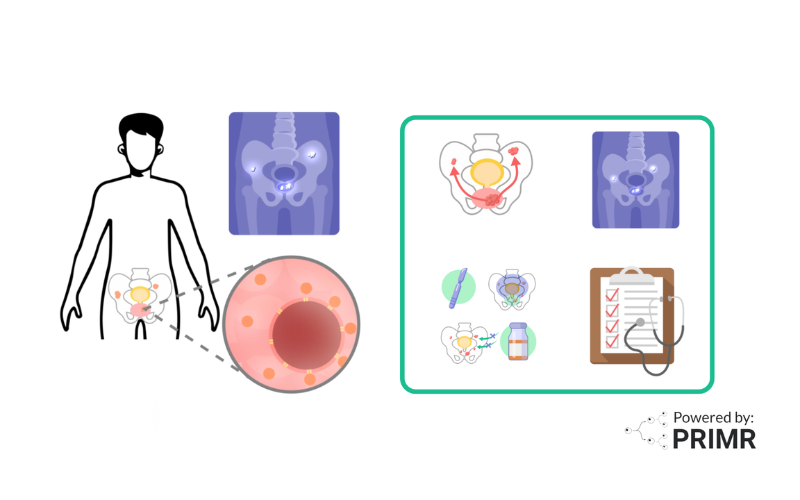
Key Applications in Cancer Care
Nuclear medicine has transformed how we diagnose and treat cancer. Some important roles include:
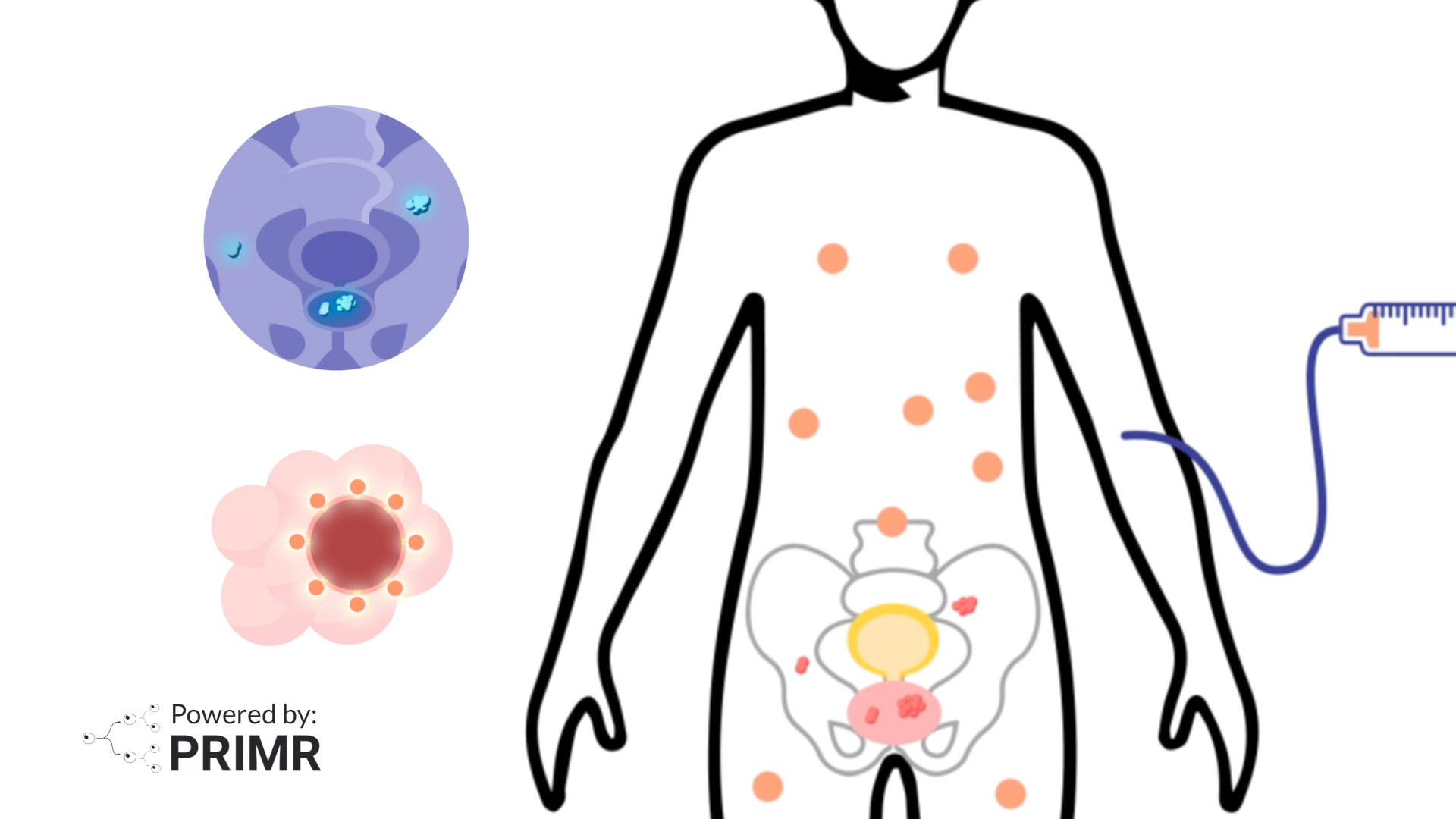
- Detection and staging of cancer: By highlighting areas where cells are unusually active, nuclear medicine can identify tumors earlier and reveal whether cancer has spread.
- Treatment planning: If we know exactly where cancer is active, we can tailor treatment strategies with greater accuracy.
- Monitoring response to therapy: Comparing scans before, during, and after treatment allows us to see whether a treatment is effective and make changes if necessary.
- Therapeutic application: One of the most promising areas of nuclear medicine is Radioligand Therapy (RLT). Unlike chemotherapy, which affects both healthy and cancerous cells, RLT delivers radiation directly to cancer cells that carry specific protein targets. This precision reduces the impact on healthy tissues and offers patients a treatment that is both targeted and potentially better tolerated.
Why Nuclear Medicine Matters for Research and Patients
Nuclear medicine is not just about improving imaging, it’s about shaping the future of cancer care. Researchers are developing new radiotracers to target a wide range of cancers, from prostate to lung. For instance, in trials like CLARIFY, we are exploring agents that could detect even smaller clusters of cancer cells, helping doctors make treatment decisions with more confidence.
For patients with lung cancer, this is especially meaningful. Accurate imaging can be the difference between catching the disease early, adjusting treatment at the right time, or even finding new therapeutic targets that weren’t visible before. As trials confirm the value of new radiopharmaceuticals, they could redefine standards of care worldwide.
—
Nuclear medicine represents a powerful bridge between diagnosis and treatment—helping doctors not only see cancer more clearly but also deliver therapy directly to where it’s needed most. For patients, it means earlier detection, more precise treatments, and potentially fewer side effects.
As research continues to advance, I remain hopeful that nuclear medicine will open even more doors for patients—particularly those with lung cancer—offering them better outcomes and more reasons to hope for a healthier tomorrow.
To learn more about Nuclear Medicine, watch the video we made here.
To learn more, browse our library of nuclear medicine and prostate cancer-related topics.
Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
Could nuclear medicine scans replace standard imaging like CT or MRI in the future?
Right now, nuclear medicine doesn’t replace CT or MRI but often works alongside them. CT and MRI show the structure of the body—like the size or shape of a tumor—while nuclear medicine shows function, such as how active the cancer cells are. In many cases, doctors actually combine the scans, like in PET/CT, which overlays both types of information for a clearer picture. While it may not fully replace traditional imaging, nuclear medicine is making diagnoses more precise and reducing the chances of missing hidden disease.
What kinds of cancers benefit most from nuclear medicine right now?
Nuclear medicine is especially useful in cancers where early detection of spread changes treatment plans. For example, prostate cancer often uses PSMA PET scans to detect very small clusters of disease that don’t show up on CT scans. In lung cancer, nuclear imaging can help determine if suspicious spots are active cancer or scar tissue. In lymphoma, it helps measure whether treatment is working, sometimes even before physical shrinkage of the tumor happens. These examples show how nuclear medicine directly impacts decisions about surgery, chemotherapy, or radiation.
Are there risks to repeated nuclear medicine scans, especially from the radiation exposure?
The radiation from nuclear medicine is generally low and carefully monitored, often comparable to or slightly higher than a standard CT scan. Most tracers are designed to leave the body quickly, which helps limit long-term exposure. For patients with cancer, the benefits of getting a more accurate diagnosis or staging usually outweigh the small risks of radiation. Still, doctors avoid unnecessary scans and only recommend nuclear imaging when it adds valuable information that could guide treatment. Ongoing research is also developing tracers with shorter half-lives and lower radiation doses to make the process even safer.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care