The ARCHER Study and a New Path for Bladder Cancer Treatment

By: David Grew MD MPH
"...carefully targeted, high-dose radiation delivered in fewer treatments can be both safe and effective."
∗ ∗ ∗
As a radiation oncologist, one of the most common questions I hear from patients is: “Do I really need my bladder removed, or is there another way to treat this?” It’s an important and very personal question, because for patients with muscle-invasive bladder cancer (MIBC), the traditional approach often involves surgery to remove the bladder entirely. While surgery can be effective, it also has life-altering consequences.
This is where new research becomes so critical. The ARCHER clinical trial is testing whether a different way of delivering radiation, more precise, shorter, and potentially less burdensome, could provide the same cancer control as the longer, more conventional treatment.
If successful, the trial could reshape how we approach bladder cancer treatment and give patients more options for both survival and quality of life.
Understanding Muscle-Invasive Bladder Cancer (MIBC)
When bladder cancer spreads into the muscle layer of the bladder wall, it becomes what we call muscle-invasive bladder cancer. At this stage, the disease carries a higher risk of spreading to other parts of the body. Without effective treatment, it can progress quickly.
Traditionally, doctors have recommended bladder-preserving therapy, which combines chemotherapy and radiation therapy. Chemotherapy helps weaken or kill cancer cells throughout the body, while radiation directly targets and destroys cancer in the bladder. The goal is to control the disease while allowing patients to keep their bladder.
However, while effective, standard radiation usually requires daily treatments for about four to six weeks, which can be challenging for patients and still comes with side effects like fatigue, bladder irritation, or bowel changes.
What Makes ARCHER Different
The ARCHER trial is testing whether a newer technique called stereotactic body radiation therapy (SBRT) can offer the same effectiveness as standard radiation, but with far fewer treatment sessions.
Unlike conventional radiation, which spreads treatment over 20 daily sessions in four weeks, SBRT delivers very precise, high doses of radiation in just five treatments within that same timeframe. This approach, also known as ultra-hypofractionation, may not only be more convenient but could also better protect nearby healthy tissues thanks to advances in planning and imaging technologies.
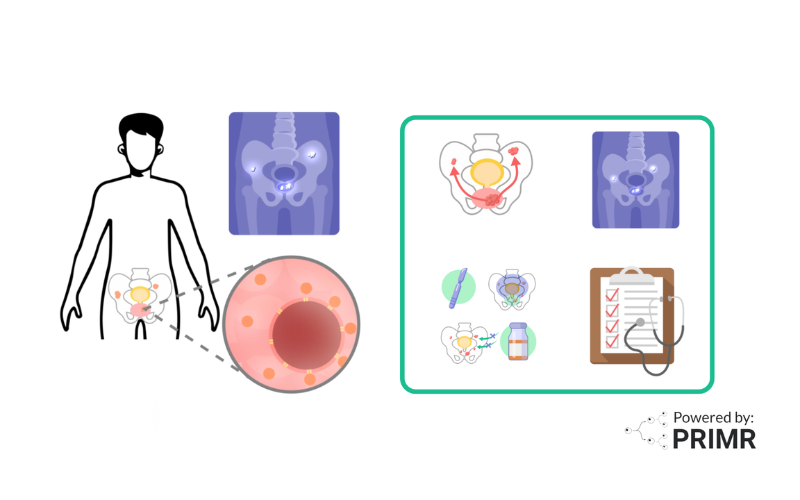
Patients in the trial are randomly assigned to one of two groups:
- Standard arm: chemotherapy with daily radiation (about 20 sessions).
- SBRT arm: chemotherapy with SBRT (just 5 sessions).
Both groups receive the same four weeks of chemotherapy. What’s being tested is whether fewer, more powerful radiation sessions can match the outcomes of the traditional approach.
Adding Modern Tools: Urine and ctDNA Testing
Beyond comparing radiation schedules, the ARCHER trial is also integrating advanced monitoring tools. One of the most exciting is the use of circulating tumor DNA (ctDNA) testing.
When cancer cells die, they release fragments of DNA into the bloodstream. By measuring ctDNA, doctors may be able to detect early signs of recurrence long before tumors appear on scans. Alongside ctDNA, urine testing will also be used to monitor for bladder cancer recurrence, providing a more complete picture of how well treatments are working.
This combination of advanced imaging, precision radiation, and molecular monitoring represents a modern, comprehensive approach to bladder cancer care.
Why This Study Matters
The primary goal of ARCHER is to see whether patients can achieve the same long-term cancer control with a shorter, more convenient course of treatment. If proven effective, SBRT could:
- Reduce the number of hospital visits.
- Minimize side effects.
- Improve patient quality of life.
- Allow more patients to preserve their bladder.
Equally important, the integration of ctDNA monitoring could help doctors intervene earlier if cancer returns, giving patients a better chance at long-term survival.
–
Trials like ARCHER are about more than testing new technologies. They’re about rethinking how we care for patients. For those living with bladder cancer, the possibility of effective treatment that is shorter, less disruptive, and bladder-preserving is deeply meaningful.
And for patients with lung cancer, where SBRT is already a proven tool, the results of ARCHER could reinforce what we already know: that carefully targeted, high-dose radiation delivered in fewer treatments can be both safe and effective. Each successful trial adds to the growing body of evidence that precision radiation can transform cancer care across different diseases.
I am hopeful that studies like ARCHER will continue to push the field forward—not only offering new treatment possibilities for bladder cancer but also strengthening our strategies for other cancers like lung cancer. Every step in research brings us closer to a future where treatments are not just effective, but also more patient-centered.
To sign up, or to learn more about the ARCHER clinical trial, watch the video we made here.
To learn more, browse our library of bladder cancer-related topics. To learn more about ctDNA testing, browse these links: Circulating Tumor DNA and the Signatera test.
Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
Could SBRT have different long-term side effects compared to standard radiation?
Because SBRT gives higher doses of radiation in fewer treatments, some people wonder if that means stronger side effects. In other cancers, like lung cancer, SBRT has been shown to be safe, though some patients do notice bladder irritation, bowel changes, or long-term urinary symptoms. The ARCHER trial is designed to see if SBRT can keep these side effects as low as, or even lower than, the longer standard treatment, while still controlling the cancer.
How reliable is ctDNA testing in bladder cancer compared to traditional scans?
CtDNA testing is an exciting new tool because it can sometimes spot cancer coming back months before a scan shows anything. That gives doctors a chance to act earlier. It’s not perfect, though—sometimes results can suggest cancer when it’s not there or miss it when it is. That’s why in ARCHER, ctDNA is being used together with scans and urine tests, to give the clearest picture possible.
What happens if cancer comes back after SBRT?
If cancer does return after SBRT, there are still good treatment options available. Some patients may go on to surgery, while others may get medicines like immunotherapy or additional treatments depending on where the cancer shows up. A big advantage of the trial is that patients are closely monitored with ctDNA and urine tests, so if the cancer does return, doctors can find it early and move quickly with the next best treatment.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care