Oligometastatic Prostate Cancer and the METANOVA Trial
).png)
By: David Grew MD MPH
"In the exciting new METANOVA study, patients with oligometastatic prostate cancer get standard hormone therapy and radiation to the prostate with or without stereotactic radiation to all sites of metastatic disease elsewhere in the body."
∗ ∗ ∗
With wider adoption of PSMA PET CT, physicians are discovering more prostate cancer patients with oligometastatic disease. Oligometastatic disease means cancer has spread from the prostate to only a few other sites in the body.
There is still some debate among doctors about precisely how many sites of disease qualify as oligometastatic. However, everyone agrees on the concept that there may be some patients where even though cancer has spread, it is potentially still curable (or at least we're able to control it for a long time) with aggressive treatment to all sites of spread.
For oligometastatic prostate cancer, prior studies have shown that some men with oligometastatic disease benefit from radiation treatment to the prostate, even though cancer has spread elsewhere.
In the exciting new METANOVA study, patients with oligometastatic prostate cancer get standard hormone therapy and radiation to the prostate with or without stereotactic radiation to all sites of metastatic disease elsewhere in the body.
We made this IRB approved video to spread the word among physicians, and to help patients understand the trial in lay language with simple visuals.
You can read the patient-centric video script below:
This video is an overview of a new clinical trial for men with oligometastatic prostate cancer who have been treated with long-term hormone therapy.
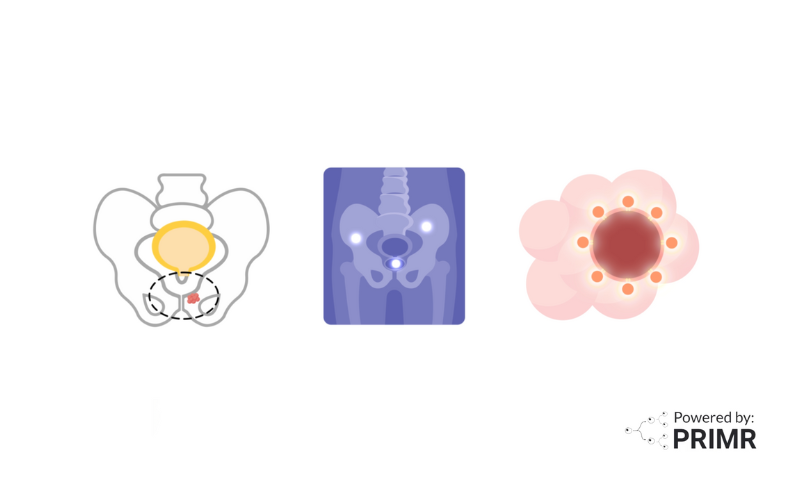
When prostate cancer spreads outside the prostate to bones or other organs, it is called metastatic prostate cancer.
Doctors can count the number of metastatic spots seen on scans. When there are only a limited number of spots, it is called oligometastatic prostate cancer.
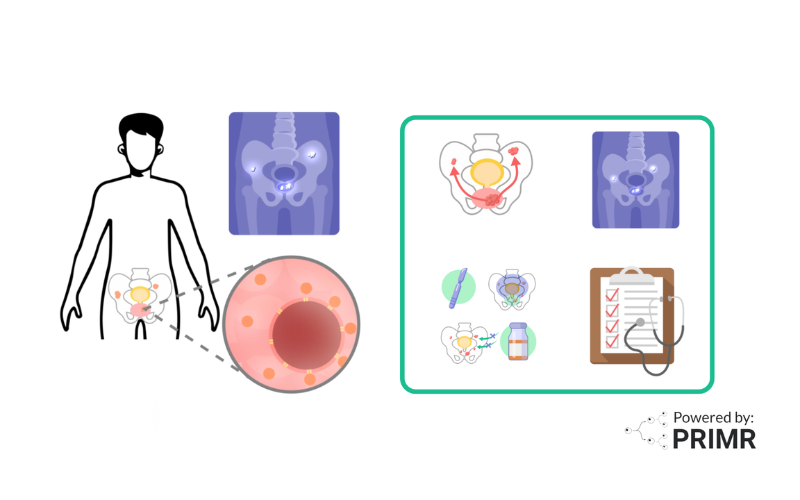
The current standard treatment for patients with oligometastatic prostate cancer is systemic therapy and treatment to the prostate.
Standard systemic therapy includes hormone therapy. Hormone therapy means drugs that prevent testosterone from fueling growth or prostate cancer. Hormone therapy can slow or stop the growth of oligometastatic prostate cancer.
Prostate treatment can be done with radiation. Radiation is non-invasive high energy x-rays targeted at cancer in the prostate.
In the past, radiation treatments for oligometastatic prostate cancer were mainly aimed at improving quality of life.
But, recent studies suggest that patients with oligometastatic disease may benefit from treating all sites of disease with radiation. This is called metastasis directed radiotherapy or MDRT. MDRT uses highly targeted radiation to each site of metastasis. Studies have shown MDRT extends the time until cancer returns and may help some patients live longer
A key question is whether adding MDRT to standard systemic therapy and prostate directed treatment can extend the time until prostate cancer grows back or make patients live longer.
In this clinical trial, participants are randomly assigned to receive either the standard treatment with systemic therapy and prostate directed treatment, OR systemic therapy, prostate treatment AND MDRT to all sites of metastasis.
Patients can enroll on this trial if they have up to 10 sites of oligometastatic disease.
The study is open label, which means that the participants and researchers will know which treatment each participant is receiving.
After treatment, all participants will be followed by doctors for routine testing to see how cancer responded to treatment.
The primary benefit of enrolling on this trial is helping patients in the future receive more effective treatment for oligometastatic prostate cancer. Another potential benefit is that very few patients off trial would get MDRT to all sites of oligometastasis, especially when up to 10 are present. This may improve patient outcomes in regards to tumor control as well as quality of life by preventing these areas from causing problems later.
To learn more about the study, talk to your doctor or click the link shown here.
FAQs:
What criteria define the "limited number of spots" to diagnose oligometastatic prostate cancer, and is there a consensus among specialists?
This varies among specialists, but it generally refers to cancer that has spread to a few, typically three to five, distinct locations outside of the prostate. The exact number can differ based on the criteria used in various studies or clinical practices, and there isn't a universally accepted threshold. However, the concept revolves around the idea that a more targeted and aggressive treatment approach could be beneficial when the disease has spread to a limited number of sites. On this trial, when PSMA-PET staging is done, participants can have up to 10 spots.
What are the potential side effects or risks associated with undergoing MDRT (metastasis-directed radiotherapy), especially when targeting up to 10 sites of metastasis?
This can vary depending on the locations of the metastases, the total radiation dose, and the patient's overall health. Common side effects could include fatigue, skin reactions in the treated areas, and mild to moderate pain or discomfort. More specific risks can be related to the sites being treated; for example, radiation to bone metastases might increase the risk of fractures, while treatment of metastases in or near organs could potentially impact organ function. The METANOVA study aims to closely monitor participants for any adverse effects to ensure the therapy's safety and efficacy.
How will the effectiveness of MDRT in extending patients' lifespans be measured throughout the METANOVA study?
This will be measured by comparing the outcomes of participants who receive standard treatment with those who receive the added MDRT. Key metrics will include overall survival rates, progression-free survival (the length of time during and after treatment that a patient lives with the disease without it getting worse), and quality of life. These outcomes can provide valuable insights into whether targeting all sites of metastasis offers a significant benefit over the standard approach.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care