A New Direction for Lung NETs: Exploring the Alliance Study and Lutetium Therapy
By: David Grew MD MPH
"The potential impact is significant: better tumor control, improved quality of life, and a more hopeful outlook..."
∗ ∗ ∗
As a radiation oncologist, I often care for patients facing complex and rare cancers. For diseases like NETs, standard treatments like everolimus targeted therapy may eventually stop working. In other cases, the side effects are simply too much. When this happens, doctors and patients are faced with difficult decisions about next steps.
The Alliance for Clinical Trials is conducting a new study exploring whether a targeted radiation treatment called Lutetium 177 Dotatate can offer better results than the current standard drug, everolimus, for patients with advanced lung NETs. The findings could significantly expand treatment options for a group of patients with few effective therapies today.
Understanding Advanced Lung NETs
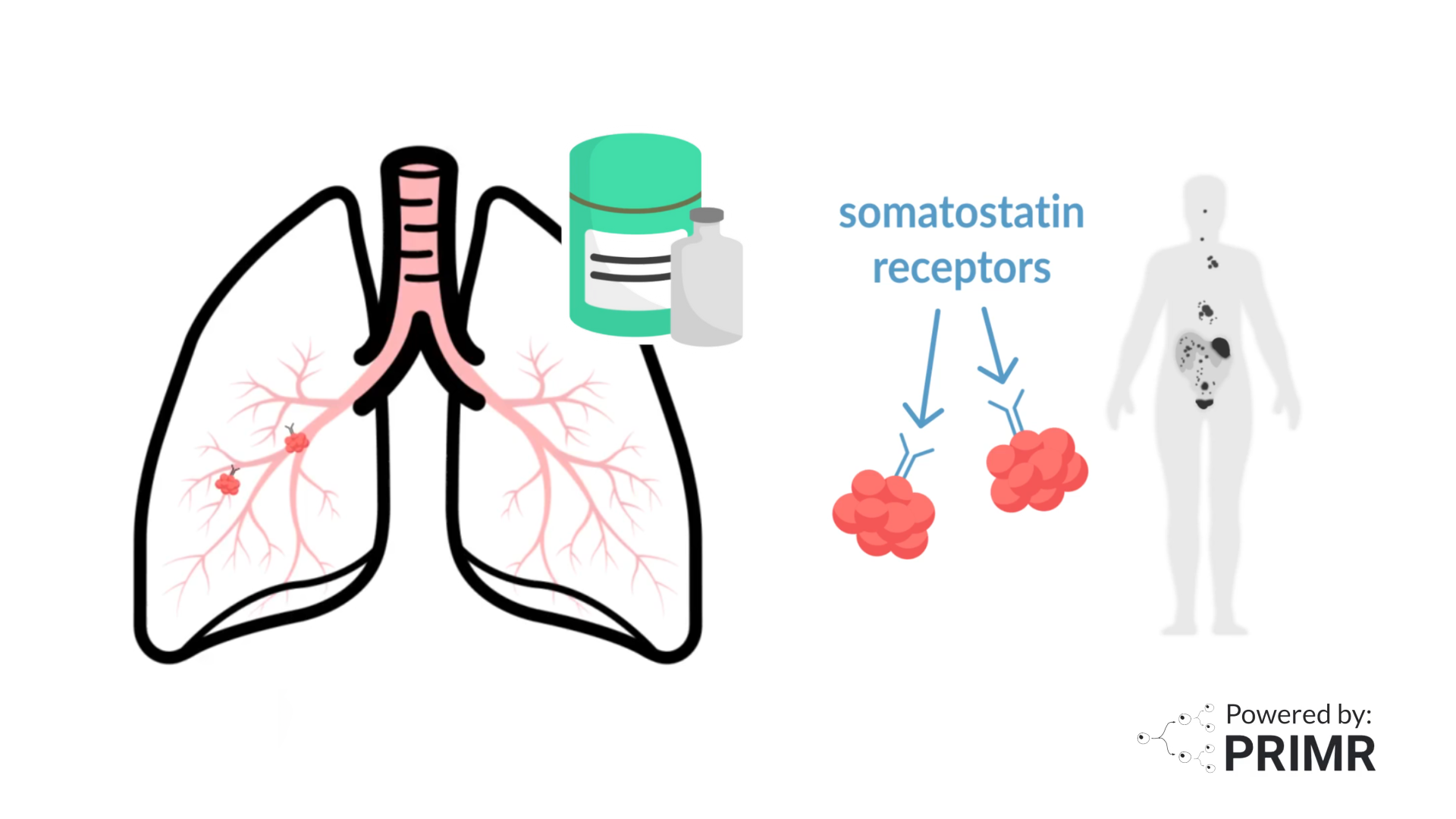
Lung NETs are a rare type of tumor that starts in the lungs but behaves very differently from more common forms of lung cancer. While some NETs grow slowly, they can still spread, often to the liver, bones, or lymph nodes. When that happens, they are considered advanced, but they are often still treatable.
One key feature of many lung NETs is the presence of somatostatin receptors on the tumor surface. These receptors can be identified through a specialized PET scan, which helps doctors know if a patient is a good candidate for certain targeted treatments, like the one being tested in this study.
Current Treatment Challenges
Right now, the only approved treatment for advanced lung NETs is everolimus, a pill that works by slowing the growth of cancer cells.
While it can be effective, it is far from perfect. Not all patients respond to it, and even when they do, the cancer often becomes resistant over time. Some patients also stop treatment because of side effects. So, while everolimus is useful, it does not meet the needs of every patient.
This is why researchers are looking into Lutetium 177 Dotatate, a treatment that is already approved for other types of NETs (like those originating in the gastrointestinal tract). Now, they want to see if it could also work for patients with lung NETs.
How Lutetium Therapy Works
Lutetium 177 Dotatate is a type of radioligand therapy. It combines a small molecule that specifically targets tumor cells (thanks to those somatostatin receptors) with a radioactive isotope called Lutetium-177.
The molecule finds the cancer, and the radiation delivers a focused attack, minimizing damage to surrounding healthy tissues.
This kind of targeted approach has already been shown to help in other NETs.
Inside the Alliance Lung NETs Trial
This study compares Lutetium 177 Dotatate directly to everolimus in patients whose tumors have somatostatin receptor uptake. To keep things fair and unbiased, patients are randomly assigned to one of the two treatments.
In the Lutetium group, patients receive the drug as an intravenous infusion every 8 weeks, for up to four doses, unless the cancer worsens or side effects become too difficult.
In the Everolimus group, patients take a daily pill continuously until disease progression or intolerable side effects.
Because this is an open-label study, both the patient and the doctor will know which treatment is being given. Throughout the trial, participants undergo regular scans and lab work to assess how their tumors are responding and to monitor for side effects.
Why This Study Could Be a Turning Point
If Lutetium proves to be more effective or even better tolerated than everolimus, it could open the door to a new standard of care for patients with advanced lung NETs. It could also offer more personalized options, especially for patients whose disease is progressing or who have struggled with side effects from current therapies.
The potential impact is significant: better tumor control, improved quality of life, and a more hopeful outlook for people with this uncommon and often under-researched cancer.
–
Lung NETs can be unpredictable, but the research community is actively working toward better treatments, and this trial is a promising example. For patients and families navigating this diagnosis, it’s reassuring to know that new therapies are on the horizon.
To learn more about the Alliance Lung NETs clinical trial, watch the video we made here.
To learn more, browse our library of lung cancer-related topics.
Are you running a trial? Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
What are the possible side effects of Lutetium 177 Dotatate for patients with lung NETs?
While Lutetium 177 Dotatate is generally well tolerated in patients with non-lung NETs, it can still cause side effects. The most common include nausea, fatigue, low blood counts, and sometimes mild kidney or liver issues. Since it delivers radiation directly to tumors, there’s a lower chance of damaging healthy tissue, but long-term effects are still being studied, especially in lung NET patients. This trial will help researchers understand how safe the treatment is for this specific group.
Are there any specific health conditions that would make a patient ineligible for Lutetium treatment?
Yes, patients with severely reduced kidney function, low blood counts, or certain other medical conditions may not be eligible for Lutetium treatment due to potential risks. Since Lutetium is a form of targeted radiation, it’s important that the body can process and clear the treatment safely. The study team will review each patient’s health history and current labs to decide if this treatment is a safe option.
How is somatostatin receptor PET imaging different from regular CT or MRI scans?
Somatostatin receptor PET scans use a special tracer that binds to certain proteins found on NET cells, making it easier to spot small or hidden tumors that might not show up on regular CT or MRI scans. This scan is crucial for determining eligibility for Lutetium treatment, since it only works on tumors that “light up” with this tracer. It's a more sensitive tool for understanding where the cancer is and how active it is.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care