Preventing Chemotherapy-induced Nausea
.png)
By: David Grew MD MPH and Melissa Propfe RN OCN
"...we’ve not completely stamped out chemo-induced nausea, but we’ve certainly been able to control it better than the prior era."
∗ ∗ ∗
Since I’m only 9 years out from residency, I have mostly practiced oncology in an era where doctors have a powerful arsenal of tools to beat back chemotherapy-induced nausea. When I read The Emperor of all Maladies, I was horrified by the descriptions of how debilitatingly sick early chemotherapy regimens made patients.
In the current era (writing this in 2024), we’ve not completely stamped out chemo-induced nausea, but we’ve certainly been able to control it better than the prior era.
Cisplatin is very effective against a variety of cancers, including head and neck cancer, certain lung cancers, cervical cancer, ovarian cancer, uterine cancer and certain germ cell cancers. But despite its potent anti-cancer effect, cisplatin chemotherapy has a high chance of causing nausea.
To help patients understand how doctors use medicines both to prevent cisplatin-induced nausea, as well as to treat breakthrough nausea, we made this video.
Below you can find a patient-friendly, lay-language explanation of how we currently help patients safely get through cisplatin-induced nausea:
___
The goal with any treatment-related nausea is prevention, to decrease the chance of malnutrition or dehydration, and to preserve a person’s ability to continue participating in all daily activities, including cancer treatment.
Some chemotherapy drugs are more likely to cause nausea than others. Your medical team will customize your treatment plan to reduce the chance you experience severe nausea.
Cisplatin has a very high chance of causing nausea when no anti-nausea medication is utilized. It may occur more than 24 hours after the medication is administered. To prevent nausea, your care team may recommend nausea prevention medications prior to starting chemotherapy that could continue at home a couple days after chemotherapy infusion.
Some common nausea prevention medications include aprepitant (Emend), palonosetron (Aloxi), and dexamethasone (Decadron). Please discuss with your treatment team which medications and schedule are most appropriate for you.
There are other factors that place an individual at a greater risk of experiencing nausea including female gender, younger age, history of motion sickness, nausea with pregnancy, minimal use of alcohol, or anxiety.
What if you experience nausea during treatment even though you are using preventative medication? This may happen, and if it does you can use prescribed anti-nausea medication as needed. Common anti-nausea medications are prochlorperazine (Compazine) and ondansetron (Zofran). Compazine can be taken every 6 hours as needed and Zofran can be taken every 8 hours as needed.
It’s important to know that you will need to wait 3 days before using Zofran if Aloxi was given prior to chemotherapy administration. The reason is Aloxi is a long-acting anti-nausea medication in the same drug class as Zofran. Aloxi is better able to provide extended anti-nausea effect because it stays in your system for several days. Zofran use can begin on or after Day 4 of each chemo cycle. If nausea is difficult to control, it is acceptable to take both Compazine and Zofran on an alternating schedule every 4 hours.
Anti-nausea medications do have side effects. Zofran can cause constipation. Patients who take Zofran for an extended period of time may need to use over-the-counter stool softeners. Dexamethasone is a steroid medication that can elevate blood glucose levels. Frequent monitoring of blood sugar levels or adjustment in diabetic medication may be necessary in individuals diagnosed with diabetes. Dexamethasone may be better tolerated when taken with meals since it can also cause an upset stomach. If indigestion is a contributing factor to nausea, antacid medication may be prescribed.
In addition to using medication, changes to eating habits can also help with nausea control. Eating smaller amounts of food more frequently throughout the day may reduce nausea while still allowing for adequate calorie intake. Avoid heavy, greasy foods, or foods high in fat since they are more likely to trigger nausea. Remain upright for 2 hours after eating to allow for complete digestion. Remember to drink plenty of fluids to prevent dehydration and help preserve normal kidney function.
This is not medical advice for individual patients and is meant as an educational resource only. Talk to your doctor before making any medical decisions.
FAQs:
How does the efficacy of these anti-nausea medications compare with each other, and are there situations where one is preferred over the others based on the patient's specific condition or type of cancer?
The efficacy of anti-nausea medications like aprepitant (Emend), palonosetron (Aloxi), and dexamethasone (Decadron) may vary depending on the individual's response and the specific chemotherapy regimen. Physicians tailor the choice of medication based on factors such as the patient's medical history, type of cancer, and potential drug interactions.
Can the long-term use of these anti-nausea medications, especially steroids like dexamethasone, lead to dependency or other significant health issues?
Prolonged use of medications like dexamethasone may lead to side effects such as elevated blood glucose levels. Patients with diabetes may require closer monitoring of their blood sugar levels or adjustments in their diabetic medications. Additionally, dexamethasone may be better tolerated when taken with meals to minimize stomach upset.
How do these anti-nausea management strategies change for pediatric patients or for elderly patients who might have different sensitivities or tolerances to these medications?
Due to differences in their sensitivities or tolerances to medications, strategies may need to be modified. Pediatric doses may need adjustment based on weight or age, while elderly patients may require closer monitoring for potential side effects or drug interactions. Open communication between patients, caregivers, and healthcare providers is crucial to ensuring personalized and effective nausea management in these populations.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
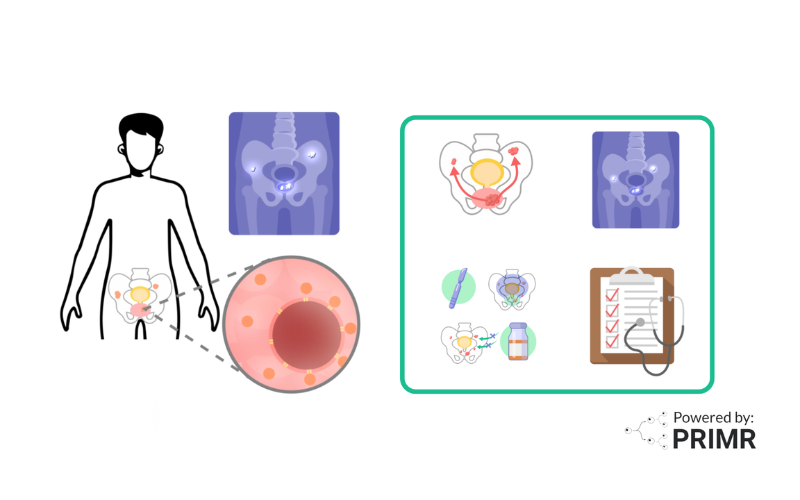
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care