What is Myelofibrosis? Essential Steps for Diagnosis, Risk Assessment, and Treatment

By: David Grew MD MPH
“In myelofibrosis, the bone marrow gradually fills with scar tissue, which disrupts the production of healthy blood cells."
∗ ∗ ∗
As a radiation oncologist, I rarely encounter myelofibrosis (MF) in my practice. However, when I recently read up on MF for a new clinical trial, I discovered several surprising aspects of this condition. MF stands out from other cancers in significant ways. Unlike most cancers that use a stage I through IV classification system, MF does not have a staging process. Additionally, while surgery and radiation are common treatments for many cancers, these approaches are not typically used for MF. To assist patients and families facing a new MF diagnosis, I've compiled a summary of other essential facts about this unique condition.
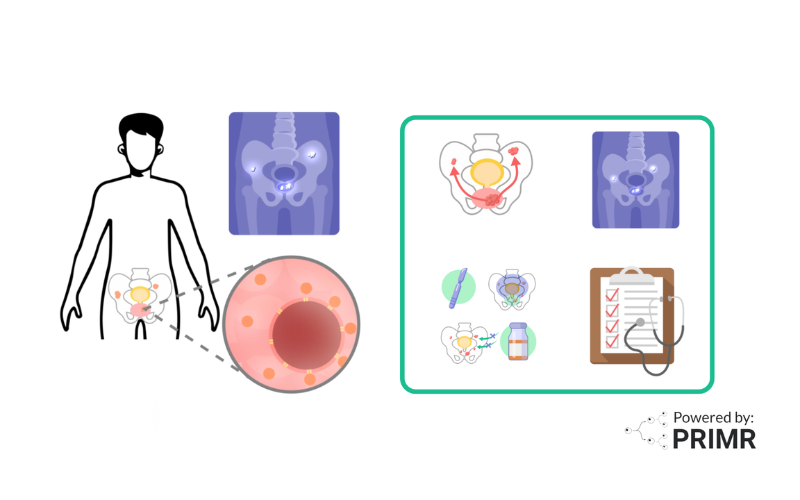
What is Myelofibrosis?
Myelofibrosis, or MF, is a rare type of blood cancer that originates in the bone marrow, the spongy tissue inside bones responsible for producing blood cells. In myelofibrosis, the bone marrow gradually fills with scar tissue, which disrupts the production of healthy blood cells. This disruption can lead to various symptoms, such as fatigue, weakness, an enlarged spleen (causing abdominal discomfort), night sweats, fever, and weight loss. Some patients may have no symptoms in the early stages, making diagnosis challenging.
Step 1: Diagnosis
Diagnosing myelofibrosis involves a series of tests that help determine if and how the disease has affected the bone marrow and blood cells.
- Blood Tests: The diagnostic process typically begins with a blood test to check for abnormal blood cell counts. Unusual results can prompt further investigation.
- Bone Marrow Biopsy: If blood tests suggest an issue, a bone marrow biopsy is often the next step. During this procedure, a small sample of bone marrow is taken, usually from the hip bone, to be analyzed under a microscope. This biopsy can reveal scar tissue or other indicators of myelofibrosis.
- Imaging Tests: Additional imaging tests, such as ultrasound or CT scans, may be used to detect an enlarged spleen or other abnormalities associated with the disease.
Step 2: Risk Assessment
Unlike many cancers, myelofibrosis doesn’t have a traditional staging system. Instead, doctors use risk scoring systems to predict the disease’s progression and inform treatment decisions.
- Scoring Systems: One common scoring system is the MIPSS70, which considers various factors such as genetic mutations, blood counts, symptoms, and bone marrow characteristics. The score helps classify patients as low, intermediate, or high risk.
- Risk-Based Approach to Treatment: For patients with low-risk myelofibrosis, doctors may recommend regular monitoring rather than immediate treatment, especially if symptoms are minimal. On the other hand, high-risk patients might require more aggressive treatment approaches.
Step 3: Treatment Options
Treatment for myelofibrosis is individualized, often based on the patient's symptoms, risk score, and overall health.
- JAK Inhibitors: JAK inhibitors are a class of medications that target signaling pathways involved in myelofibrosis progression. These drugs can alleviate symptoms, improve quality of life, and, in some cases, extend survival.
- Other Medications: In certain situations, other medications such as hydroxyurea, interferon alpha, or drugs that address anemia-related symptoms may be prescribed to help manage discomfort and improve blood cell counts.
- Stem Cell Transplantation: For patients with intermediate or high-risk myelofibrosis, especially those who are younger and otherwise healthy, a bone marrow (allogeneic stem cell) transplant offers the only potential cure. However, this option is complex and not suitable for everyone, given its risks and the demands on the patient’s health.
∗ ∗ ∗
The journey through myelofibrosis from diagnosis to treatment can feel overwhelming, but each step helps ensure that patients receive the care best suited to their individual case. By understanding the nature of the disease, knowing how risk is assessed, and being aware of treatment options, patients and their families can feel more empowered in managing this condition.
To learn more about myelofibrosis, watch the video we made here.
Hire PRIMR to create custom video content for your clinical trial or medical product today.
FAQs:
What causes myelofibrosis, and is it hereditary?
The exact cause of myelofibrosis is unknown, but it’s thought to result from genetic mutations that affect blood cell production in the bone marrow. Some patients with myelofibrosis have mutations in the JAK2, CALR, or MPL genes, which are involved in blood cell regulation. While these mutations can occur spontaneously, myelofibrosis is generally not considered hereditary and does not typically run in families. However, having a family history of certain blood disorders may increase the risk slightly.
How does myelofibrosis affect life expectancy and quality of life?
Life expectancy and quality of life for individuals with myelofibrosis vary widely based on risk factors such as age, overall health, and specific genetic mutations. Patients classified as low-risk may live many years with minimal symptoms, while those with high-risk disease may experience a more rapid progression. Symptoms like fatigue, anemia, and an enlarged spleen can significantly impact daily life. Targeted treatments, particularly JAK inhibitors, aim to improve quality of life by reducing symptoms, while stem cell transplants may potentially cure the disease in eligible patients.
Are there clinical trials for new treatments in myelofibrosis?
Yes, clinical trials are ongoing to explore new treatments for myelofibrosis, especially targeting different genetic mutations and pathways involved in the disease. Some investigational drugs aim to work alongside JAK inhibitors or to offer alternative mechanisms for symptom relief. Patients interested in participating in a clinical trial should consult their doctor to understand eligibility requirements, potential benefits, and risks associated with trial participation.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care