Metastatic Kidney Cancer and the SAMURAI Study

By: David Grew MD MPH
"However, some patients are too sick to undergo surgery, or perhaps simply don't want to have surgery. For them, the SAMURAI trial may be a good option."
∗ ∗ ∗
Many patients ask if they can have surgery on their cancer even though it has already spread, or metastasized, to other organs in the body. This question is a good one - it makes sense to try to remove the initial source of cancer. However that is usually not done for a variety of reasons. Once the tumor has spread, the disease affecting other organs is much more dangerous than cancer sitting in the organ where it started. Also, undergoing surgery may delay the start of treatments (like chemotherapy or immunotherapy) directed at controlling disease in other parts of the body.
But kidney cancer is a bit different. Studies have shown that some patients do better if the initial cancer in the kidney is removed, even though it has already spread elsewhere. Removing the primary tumor (kidney) might help in managing symptoms, reducing the tumor burden, and improving the effectiveness of other treatments such as targeted therapies or immunotherapies.
However, some patients are too sick to undergo surgery, or perhaps simply don't want to have surgery. For them, the SAMURAI trial may be a good option. In this study, patients with metastatic kidney cancer receive immunotherapy with or without targeted radiation at the cancer in the kidney.
You can see PRIMR’s IRB approved video here.
You can read the patient-centric video script below:
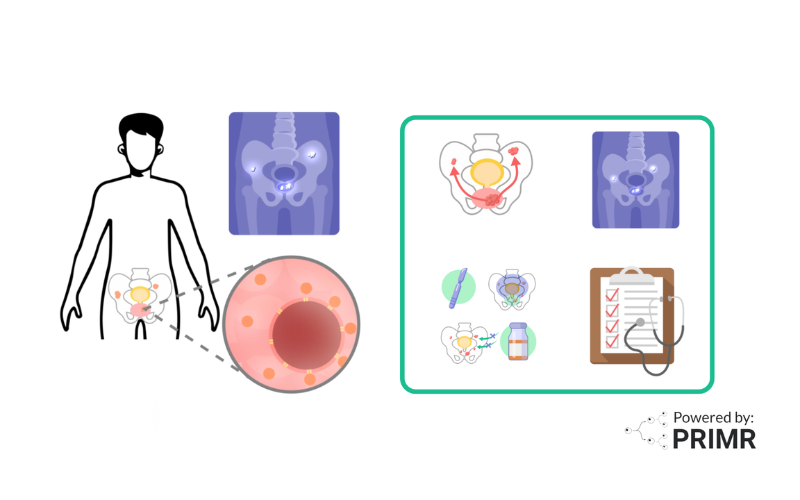
This video is an overview of a new study for patients with metastatic kidney cancer who cannot have surgery.
When kidney cancer leaves the kidney and spreads to other parts of the body, it is called metastatic kidney cancer.
The main treatment for metastatic kidney cancer is immunotherapy and antiangiogenic agents.
Immunotherapy is medication infused directly into the bloodstream. The treatment activates your own immune system to fight kidney cancer.
Antiangiogenic medications are pills taken by mouth. They stop the formation of blood vessels that bring oxygen and nutrients to the tumor. This may slow the growth and spread of the tumor.
In addition to these medications, surgery is sometimes recommended for the primary tumor in the kidney. The surgery is called a nephrectomy, and doctors remove the entire kidney. The benefits of such an operation are unknown in patients receiving immunotherapy.
Some patients are reluctant to have surgery, or they are not able to have surgery, either because the tumor is too large, or because they have other health problems that would make surgery too risky.
For these patients, minimally invasive external beam radiation therapy may be a helpful treatment for kidney cancer.
Radiation therapy is high energy x-rays targeted at the tumor in the kidney.
Radiation is delivered with high precision to protect other organs in the area.
In this study, patients who are not recommended for surgery will be randomly assigned to receive either standard immunotherapy, or immunotherapy combined with radiation.
Neither doctors nor patients decide which treatment they receive on the trial.
The study is not blinded, which means doctors and patients will know which treatments they receive.
After treatment doctors will continue to monitor patients for side effects and response to treatment.
For more information on how to enroll on this study, scan the QR code shown here.
FAQs:
What criteria are used to determine if a patient with metastatic kidney cancer is too sick for surgery?
This often involves a comprehensive assessment that includes an evaluation of the patient's overall health status, the presence of comorbid conditions, and their ability to withstand the stress of an operation. Physicians might consider factors such as cardiovascular health, pulmonary (lung) function, and other organ functions, alongside the patient's performance status, which measures their ability to carry out daily activities.
How does targeted radiation in the SAMURAI trial compare to conventional nephrectomy in terms of efficacy and safety?
Targeted radiation is not being compared to nephrectomy in the SAMURAI trial. On this trial, all participants are not eligible for nephrectomy, and no one will have surgery as part of the trial protocol. Others are exploring targeted radiation as a less invasive, therefore potentially safer, alternative to conventional nephrectomy. While traditional surgery involves removing the kidney, which can have significant recovery times and risks, targeted radiation aims to destroy cancer cells with precision, potentially offering a safer option with fewer side effects. However this trial does not compare surgery to radiation directly. Instead, the trial seeks to understand how well-targeted radiation controls cancer compared to receiving immunotherapy alone (without surgery), including impacts on survival, tumor progression, and quality of life.
What are the long-term outcomes and follow-up care plans for patients participating in the SAMURAI trial?
The trial is designed to monitor the effectiveness of the treatment, manage any side effects, and assess the impact on the patient's overall health and quality of life. Follow-up care typically includes regular medical checkups, imaging tests to monitor for cancer progression, and supportive care to address any physical or emotional health issues. The trial's findings will likely contribute to refining strategies for managing metastatic kidney cancer, potentially offering insights that help improve patient outcomes and inform future treatment protocols.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care