Multidisciplinary Care: The Driving Forces Behind Prostate Cancer Treatment

By: David Grew MD MPH
“Multidisciplinary care for prostate cancer patients ensures a holistic and coordinated approach to treatment, significantly improving patient outcomes and experiences.”
∗ ∗ ∗
When I meet patients with a new diagnosis of prostate cancer, they’re usually (understandably) overwhelmed. Not only do they need to emotionally process their first encounter with mortality, but there’s also a multitude of cutting edge treatment options to sift through. From biopsy results, to genomic tests, to PSMA PET scans, robotic surgery and stereotactic radiation - the workup and treatment options for prostate cancer have never been more complex and confusing.
Thankfully there’s a whole team of experts at the ready to help prostate cancer patients along their path to cure. But even keeping this cast of characters straight can be a source of stress. So we partnered with the team at Weill Cornell Medicine and their network of patient advocates to create a simple patient-centric video outlining the key players in multidisciplinary care.
In this blog, we'll explore the various roles involved in a multidisciplinary prostate cancer care team and how this model benefits patients.
Navigating the Journey with a Prostate Cancer Access Nurse
A prostate cancer access nurse plays a crucial role in guiding patients through their treatment journey. From the initial diagnosis to the successful completion of treatments, they help navigate appointments and gather relevant information from doctors. Their role includes:
- Initial Contact: A phone call to collect necessary information from your doctors and arrange appointments with specialists.
- Ongoing Support: Maintaining regular communication to update you on appointments, test results, and any changes in the treatment plan.
Understanding the Role of Each Specialist
Urologist
The urologist is typically the primary point of contact, orchestrating the initial diagnosis and treatment phases. They:
- Diagnose: Interpret information from general practitioners, other urologists, and imaging studies, ordering additional tests or performing biopsies as needed.
- Surgical Treatment: Perform prostatectomy surgeries for patients opting for surgical treatment.
- Active Surveillance: Coordinate monitoring for patients with lower-risk prostate cancer.
Radiologist
Radiologists play a critical role in prostate cancer care by utilizing advanced imaging techniques.
- Precise Localization: Radiologists use advanced imaging techniques like CT, MRI, and PSMA PET scans to pinpoint the exact location, size, and spread of prostate cancer.
- Tailored Imaging: They select the most appropriate imaging method based on the patient's specific condition and clinical needs, ensuring the most accurate information is gathered.
- Treatment Planning: The detailed imaging results provided by radiologists are essential for the multidisciplinary team to develop the most effective and precise treatment plans.
Pathologist
Pathologists play a vital role in diagnosing and understanding the cancer's behavior:
- Diagnosis: They analyze biopsy samples under the microscope to confirm the diagnosis of prostate cancer.
- Assessing Aggressiveness: Pathologists can estimate how aggressive the cancer may be based on tissue analysis.
- Post-Surgery Analysis: If surgery is performed, they examine the removed tissue to provide a detailed report, which may include genomic testing to tailor personalized treatment plans.
Pelvic Floor Therapist
Pelvic floor therapists play a vital role in the comprehensive care of prostate cancer patients, particularly in managing post-treatment side effects related to pelvic muscle function.
- Specialized Exercises: Teach tailored techniques for managing urinary leakage and bowel function post-treatment.
- Quality of Life Improvement: Address specific physical challenges to enhance patient well-being after treatment.
- Holistic Care Collaboration: Work closely with the multidisciplinary team to provide personalized strategies for symptom management.
Radiation Oncologist
Radiation oncologists design and implement custom treatment plans using information from biopsies and radiology scans. They:
- Treatment Planning: Develop personalized radiation therapy plans that target cancer cells with high-energy x-rays while minimizing damage to healthy tissue.
- Precision Targeting: Utilize the latest technologies to ensure radiation is delivered accurately to maximize effectiveness and reduce side effects.
Medical Oncologist
Medical oncologists oversee medical therapies, such as hormone therapy, and ensure an integrated approach to patient care:
- Therapy Coordination: Manage and coordinate medical treatments to enhance the overall treatment plan.
- Clinical Trials: Facilitate participation in clinical trials, which are essential for studying new treatments and improving outcomes and quality of life.
Additional Support Staff
- Social Workers: Provide emotional support, counseling, and help navigate the healthcare system. They assist with practical issues like transportation and financial aid.
- Nutritionists: Offer dietary guidance to help patients maintain their strength and manage side effects during treatment.
- Genetic Counselors: Assess patients' genetic risk factors and help interpret genomic testing results, aiding in personalized treatment planning.
- Patient Advocates: Serve as liaisons between patients and the healthcare team, ensuring patients' voices are heard and their needs are met.
- Other Support Staff: May include physical therapists, occupational therapists, and mental health professionals, all contributing to a holistic approach to patient care.
How can PRIMR be integrated in this approach?
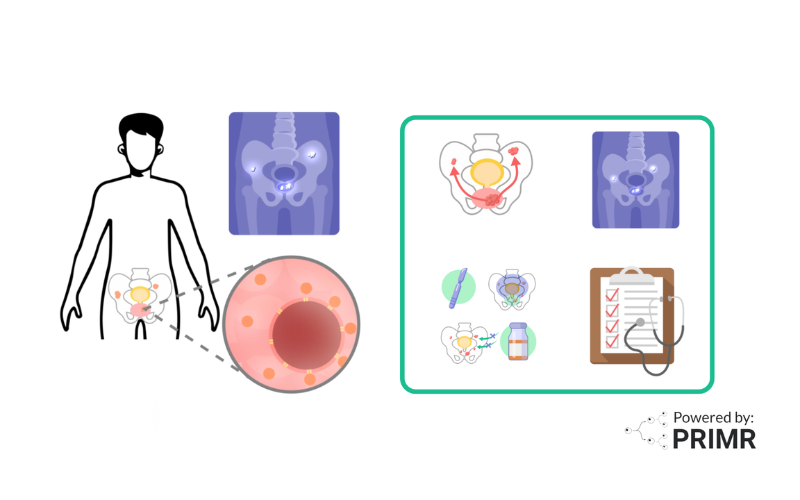
PRIMR educational videos significantly enhance patient understanding and engagement by providing a comprehensive visual overview of trial procedures and treatments. These videos ensure patients receive clear and consistent information, helping them feel empowered and confident in their treatment journey. Specifically, for prostate cancer, PRIMR has developed a video that details the multidisciplinary care process, educating patients about the roles of various specialists and preparing them for what to expect during their treatment.
These videos also enhance communication and collaboration by equipping patients with essential knowledge, allowing them to ask targeted and relevant questions. This preparation streamlines discussions, builds trust, and creates a collaborative environment. The impact is profound for both patients and researchers: patients understand expectations better, engage more proactively, and receive comprehensive care, while researchers benefit from more productive conversations, efficient information relay, and improved patient adherence to protocols, ultimately enhancing research outcomes.
∗ ∗ ∗
Multidisciplinary care for prostate cancer patients ensures a holistic and coordinated approach to treatment, significantly improving patient outcomes and experiences. Each specialist on the care team—from urologists and radiologists to pathologists and medical oncologists—plays a crucial role in diagnosing, treating, and managing the disease, while additional support staff provide essential services that address emotional, nutritional, and practical needs.
The integration of PRIMR educational videos further enhances this model by empowering patients with comprehensive, easily digestible information. These videos facilitate clearer communication, more informed decision-making, and stronger patient engagement. Together, this multidisciplinary approach and innovative educational tools create a robust support system that optimizes care and fosters a collaborative, patient-centered environment.
For more information, watch the PRIMR video on multidisciplinary care for prostate cancer and see how it can make a difference in your treatment experience.
Hire PRIMR to create custom video content for your clinical trial today.
Other Posts

Nuclear Medicine: PSMA Treatment Explained from a Doctor’s Perspective
Nuclear Medicine: PSMA Imaging and Its Impact on Prostate Cancer Care