Multidisciplinary Care for Patients with Prostate Cancer
Prostate cancer is a common cancer in men.
Discover how a diverse team of experts collaborates to enhance prostate cancer care, from precise diagnosis to tailored treatments, ensuring optimal outcomes for patients and empowering healthcare providers in delivering effective, comprehensive care.
Read the full video transcript below:
This video is an overview of multidisciplinary care for patients facing prostate cancer. This collaborative approach is designed to optimize patient outcomes and enhance the quality of care.
A prostate cancer access nurse will help navigate you through all your appointments, from the beginning of your prostate cancer diagnosis through the successful completion of treatments. They will start with a phone call to collect relevant information from your doctors and later arrange your appointments with different specialists.
Now we'll introduce you to the different types of doctors on your prostate cancer team.
First is the urologist, serving as the primary point of contact and orchestrating the initial phases of diagnosis and treatment. Urologists interpret key information from the patient, general practitioners, other urologists, and imaging studies such as CT scans or MRIs. If necessary, they will order additional tests or perform a prostate biopsy to establish a diagnosis of prostate cancer.
For patients who choose treatment with surgery, urologists who specialize in cancer (urologic oncologists) perform surgery to remove the prostate. This surgery is called a prostatectomy.
For patients with lower-risk prostate cancer, urologists will coordinate the process of active surveillance to monitor these cancers.
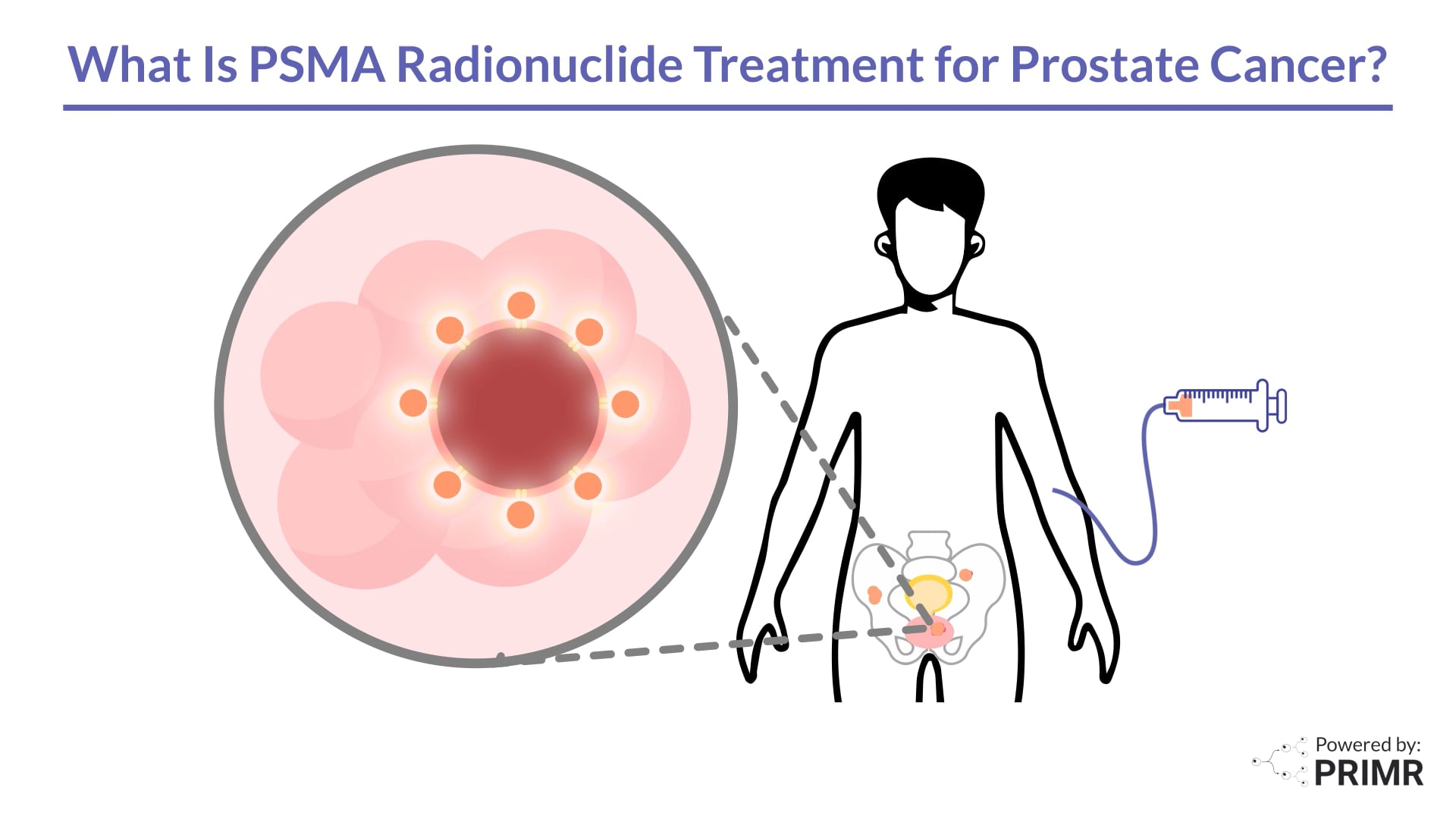
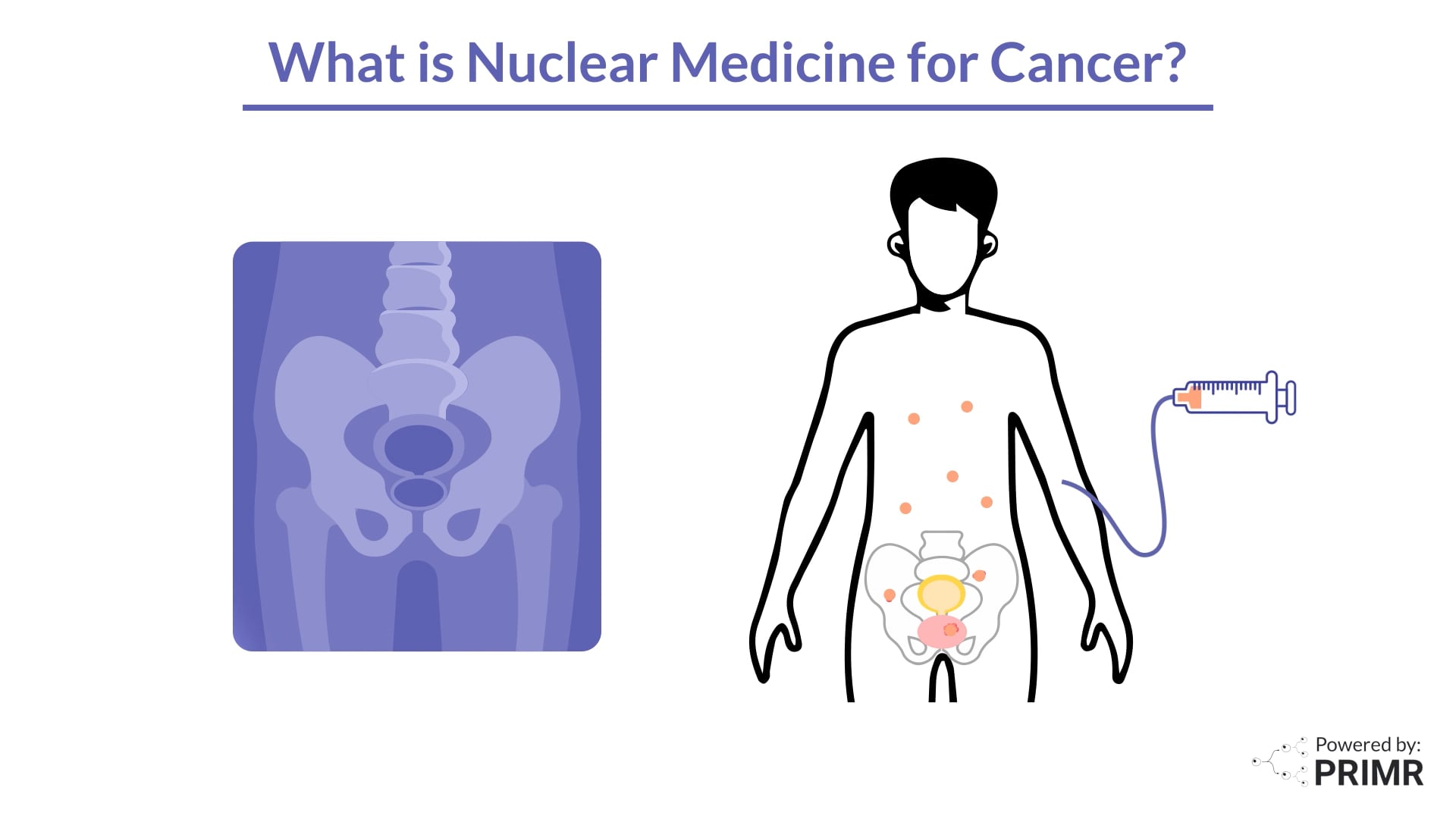
The radiologist uses advanced body imaging techniques like CT, MRI, and PSMA PET scans to tell the team where the cancer is located, how big it is, and whether it has spread to other parts of the body. This helps your team decide the best treatment for your cancer with precision and accuracy.
Next, we turn our attention to the pathologists, doctors who analyze biopsy samples under the microscope. They confirm your diagnosis of prostate cancer and can estimate how aggressive your cancer may behave.
If you have surgery, they will analyze the tissue removed and describe the features and patterns of the cancer in a report. Your treatment team may send pathology samples for additional testing, like genomic testing, to better guide treatment recommendations.
Genomic testing looks at the cancer's DNA to find specific changes that might predict how the cancer will grow or respond to treatments. This information can help tailor treatment plans, making therapy more personalized and potentially more effective.
When someone has prostate cancer, treatments like surgery or radiation can weaken pelvic muscles, leading to problems like urine leaking or difficulty controlling bowel movements. The pelvic floor therapist teaches special exercises and techniques to strengthen these muscles, helping to reduce or manage these issues. Think of them as helping you regain control and improve the quality of your daily life after prostate cancer treatment.
The radiation oncologist pulls together the information from the biopsy and radiology scans to design a custom treatment plan. Some patients will choose to undergo radiation therapy. For them, the radiation oncologist uses high-energy x-rays to directly target cancer cells while minimizing harm to healthy tissue.
Lastly, the medical oncologist coordinates any medical therapies, such as hormone therapy, ensuring a comprehensive and integrated approach to patient care. Once your team discusses your case, you may be offered participation in a clinical trial. Clinical trials are essential to safely study new treatments and improve prostate cancer outcomes and quality of life during and after treatment.
If you have any questions along the way, you can contact your prostate cancer access nurse, who will answer your questions or put you in touch with the correct physician. Additional members of your team may include social workers, nutritionists, genetic counselors, patient advocates, or other support staff.
In conclusion, this multidisciplinary care model is collaborative healthcare dedicated to empowering patients and achieving excellence in prostate cancer management.
FAQs:
How does the prostate cancer access nurse communicate updates and progress to the patient throughout their treatment journey?
The prostate cancer access nurse communicates updates and progress to the patient throughout their treatment journey by maintaining regular contact, either through phone calls or in-person meetings, to provide information about appointments, test results, and any changes in the treatment plan. They also serve as a liaison between the patient and the medical team, ensuring that the patient understands their treatment options and has access to the necessary resources and support.
How frequently will a patient meet with each type of specialist during their prostate cancer treatment?
The frequency of meetings with each specialist varies depending on the patient's specific case and treatment plan. Typically, a patient may meet with their urologist and radiation oncologist more frequently during the initial diagnosis and treatment planning stages. Follow-up visits with the urologist, radiation oncologist, and medical oncologist may occur periodically throughout treatment and during post-treatment surveillance to monitor progress and manage any side effects.
Are there any support services available for managing the emotional and psychological impact of prostate cancer diagnosis and treatment, and how can patients access these services?
Support services for managing the emotional and psychological impact of prostate cancer diagnosis and treatment are available and can be accessed through various means. These services include counseling, support groups, and mental health professionals such as psychologists or psychiatrists. The prostate cancer access nurse or social workers on the multidisciplinary team can help connect patients with these resources, ensuring they receive comprehensive care that addresses both physical and emotional well-being.

.jpg)
.jpg)
%20Thumbnail.png)




.jpg)
.png)

.jpeg)









.webp)

